Last updated on April 29th, 2023 at 11:35 pm
Pressure Ulcer Nursing Care Plans Diagnosis and Interventions
Pressure Ulcer NCLEX Review and Nursing Care Plans
Pressure ulcers, sometimes called bedsores or Decubitus ulcers, are skin and tissue breakdown that arises from exertion of incessant pressure to the skin. Continuous stress to the skins’ integrity will eventually cause skin breakdowns.
The development of pressure ulcers is an example of such skin damage. The most common sites of injuries are the bony prominences of the body, such as the heels, knees, elbows, and sacrum.
There are different stages of pressure ulcers in terms of severity. Not all stages of pressure ulcers present with open sores. The National Pressure Injury Advisory Panel (NPIAP) has coined that the most appropriate term should be “pressure injuries”.
Problems on mobility, poor nutrition, among others, predispose patients in having this condition.
Signs and Symptoms of Pressure Ulcer
The general clinical manifestations of pressure ulcers include:
- Unusual skin color or texture discrepancies
- Erythema or redness
- Edema or swelling in the affected area or limb
- Discharges – foul in odor, can be fluid or pus-filled
- Warm or cold to touch – An area of the affected region that feels different to touch than surrounding areas
- Tenderness and pain on site
Causes and Risk Factors of Pressure Ulcer
Pressure ulcers are caused by relentless pressure against the skin, thereby limiting blood flow to the skin and its surrounding tissues.
Inactivity and limited movement, particularly on bed-ridden patients, makes the skin vulnerable for the development of pressure ulcers.
There are three contributing factors for its development, and they are:
- Pressure. Constant pressure on any part, specifically on the skin of the bony prominences of the body, will lessen the blood supply to the tissues. This lack of blood supply will deprive the tissues of needed nutrition from the circulation, and in turn, will cause damage and injury to the body.
- Friction. Friction happens when the skin is rubbed against clothing, making the skin more fragile and vulnerable to injury. This is especially true if the skin is moist.
- Shear. Shear occurs when two surfaces move away from opposite directions. This action complicates the damage incurred from pressure ulcers.
The risk factors of pressure ulcers are the following:
- Immobility – may be due to poor conditions, such as spine injuries
- Incontinence – skin breakdown is more apparent with prolonged exposure to excreta and urine.
- Lack of sensory perception – problems with tactile and pain receptors from medical conditions (e.g., spinal cord injuries), will delay the response to early warning signs of skin breakdown.
- Poor nutrition and hydration – inadequate supply fluid and improper nutrition will prevent the body from healing properly and will therefore aggravate the condition.
- Medical conditions affecting blood flow – diabetes makes the blood slower to circulate, thereby delaying the risking the tissues to damage.
Complications of Pressure Ulcer
Complications of pressure ulcers are debilitating, some even life-threatening:
- Cellulitis. An infection of the skin, connective tissues and its surrounding soft tissues. It is characterized by swelling, erythema and warmth in the affected area.
- Osteomyelitis. Osteomyelitis or Bone infections are severe infections that have burrowed deeper into the bones of the body, causing damage. The damage brought by this infection will limit the mobility and functions of the affected bones.
- Cancer. Marjolin’s ulcer, a type of long-term and non-healing wound, may develop into squamous cell cancer.
- Sepsis. Severe complication of decubitus ulcer arising from overwhelming infection of wounds that compromises the hemodynamic stability of the body.
Diagnosis of Pressure Ulcer
- Medical History – Comprehensive medical history will be collected to assess extent of injury and address factors that contributed for its development. History of pressure ulcers, the type of assistance needed by the patient, and inquiries about ADL’s are some of the focus questions in history taking.
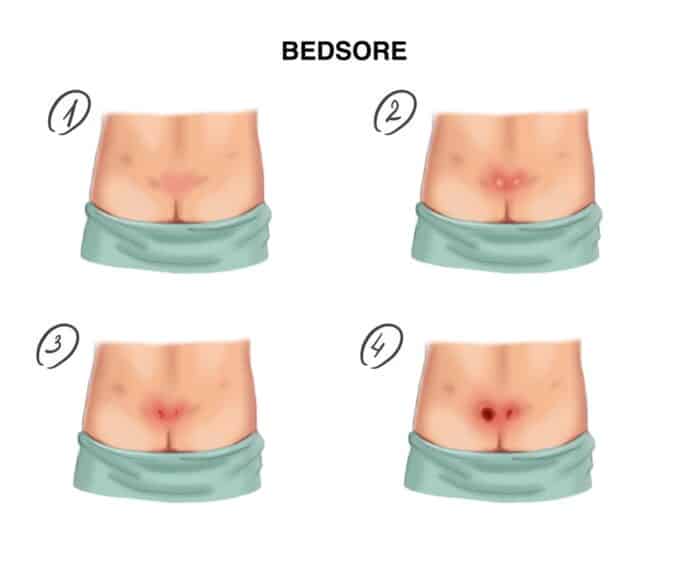
- Physical Examination – Assessing the affected area is the primary method in diagnosing decubitus ulcers. The NPIAP staging system are as follows:
- Stage 1 – intact skin with a localized area of nonblanchable erythema; may appear differently pigmented from surrounding tissue. Color changes does not involve purple or maroon discoloration.
- Stage 2 – partial thickness with skin loss and exposed dermis that is either pink or red, usually moist; may also be intact or ruptured blister; fat and muscles not visible; zero presence of slough and eschar.
- Stage 3 – full thickness with skin loss; fat tissue is exposed; granulation observed surrounding the injury; depth may vary depending on location; muscle and other connective tissue not observed; undermining and tunneling of injury may be observed.
- Stage 4 – full thickness with skin and tissue loss; exposed fascia, muscle and bone is observed; Slough or eschar is observed; undermining and tunneling of injury occurs.
- Unstageable – full thickness skin and tissue loss is observed, however extent of damaged cannot be assessed due to eschar or slough.
- Deep tissue injury – with intact or non intact skin; with localized and persistent non-blanchable deep red, maroon or purple discoloration; may have separation skin structures revealing a dark wound bed or blood-filled blister.
- Laboratory studies – These tests will be ordered to assess extent of damage and general health of the patient.
- CBC – baseline lab works to assess for infection (elevated WBC and ESR rate will mean inflammation or infection)
- Albumin, Prealbumin, transferrin and serum protein levels – to assess for the nutritional status for adequate wound healing once wound debridement is done.
- Urine and culture – to assess causes of urinary incontinence.
- Stool exam – to detect causes of diarrhea, e.g. C. difficile infection
- Blood cultures – to assess for presence of sepsis
- Imaging studies – to assess depth of injury to tissues, especially the muscles and bones.
- Biopsy – biopsy of chronic wounds may be done to rule out malignancies.
Treatment for Pressure Ulcer
- Reduction of pressure. The first step for treating pressure ulcers is to reduce further damage caused by pressure. This can be achieved through:
- Repositioning – perform frequent bed turning for bed-ridden patients every 2 hours.
- Using support equipment – examples are alternating mattresses, use of pressure-relieving or “air” mattress, and use of trochanter rolls on bony prominences.
- Physical therapy – encouraging the patient to move from bed to chair and to perform appropriate exercises through physical therapy
- Cleaning and dressing wounds. This will depend on the stage and extent of the pressure injury.
- Cleaning – for unbroken skin, a mild cleanser is used to wash then patted dry; for open sores, saline irrigations may be done after each dressing change.
- Putting bandages – bandages are helpful to protect the affected area. They will be on various forms like films, foams, etc.
- Referral to Tissue Viability Nurse team. These nurses specialize in helping to properly stage the decubitus ulcers and to suggest appropriate dressings, particularly if medicated dressings are needed.
- Debridement. This involves the surgical removal of dead and necrotic tissues to allow for new tissue to surface. This is mostly done for extensive pressure ulcers (stage 3 and 4). It may also include reconstructive surgery for the more extensive wounds and will involve the use of flaps to cover.
- Medical therapy
- Antibiotics – topical antibiotics may be required as they have excellent antimicrobial spectrum coverage
- Analgesics – anti-inflammatory drugs will be used to reduce pain, especially during dressing changes and wound care.
Nursing Diagnosis for Pressure Ulcer
Nursing Care Plan for Pressure Ulcer 1
Nursing Diagnosis: Impaired Skin Integrity related to skin breakdown secondary to pressure ulcer, as evidenced by pressure sore on the sacrum, discharge from the sores for a couple of days, pain and soreness
Desired Outcome: The patient will have optimal skin integrity by following treatment regimen for decubitus ulcers.
| Nursing Interventions for Pressure Ulcers | Rationale |
| Assess the patient’s skin on his/her whole body. Create a wound care chart. | To determine the severity and extent of decubitus ulcers and any affected areas that require special attention or wound care. |
| Commence wound care that is appropriate to the stage of the decubitus ulcer. Application of the prescribed antibiotic cream or ointment directly to the affected area may be required. | Performing the correct wound care in accordance to the stage of the decubitus ulcer maximizes the healing potential of the pressure injury. |
| Educate the carer about proper wound hygiene through washing the sores with the prescribed cleanser. Advise the patient to prevent scratching the affected areas. | It is important to maintain the cleanliness of the affected areas by washing with the prescribed cleanser. The sores may cause mild itching, but it is advisable to prevent the child from scratching the affected areas to prevent worsening of the infection. |
| Perform frequent bed turning for bed-ridden patients at least every 2 hours. Use appropriate equipment such as pressure-relieving or “air” mattress and trochanter rolls on bony prominences. | To reduce the pressure from the affected area and other bony prominences. |
| Encourage getting out of bed to sit on the chair and performing tolerable exercises. Refer to physical therapy team as needed. | Encouraging the patient to move from bed to chair and to perform appropriate exercises through physical therapy |
| If the patient is to be discharged, teach the carer the proper wound care over the affected areas. | Proper wound care and application of bandages over the affected areas can help prevent the worsening of pressure injury and promote wound healing at home. |
Nursing Care Plan for Pressure Ulcer 2
Nursing Diagnosis: Acute Pain related to pressure ulcers as evidenced by pain score of 10 out of 10, guarding sign on the affected limb, restlessness, and irritability especially during wound care
Desired Outcome: The patient will report a pain score of 0 out of 10.
| Nursing Interventions for Pressure Ulcers | Rationales |
| Assess the patient’s vital signs. Ask the patient to rate the pain from 0 to 10, and describe the pain he/she is experiencing. | To create a baseline set of observations for the patient. The 10-point pain scale is a globally recognized pain rating tool that is both accurate and effective. |
| Administer analgesics/ pain medications as prescribed, at least 30 minutes before wound care. | To provide pain relief to the patient. |
| Ask the patient to re-rate his/her acute pain 30 minutes to an hour after administering the analgesic. | To assess the effectiveness of treatment. |
| Provide more analgesics at recommended/prescribed intervals. | To promote pain relief and patient comfort without the risk of overdose. |
| Reposition the patient in his/her comfortable/preferred position. Encourage pursed lip breathing and deep breathing exercises. | To promote optimal patient comfort and reduce anxiety/ restlessness. |
More Nursing Diagnosis for Pressure Ulcer
Nursing References
Ackley, B. J., Ladwig, G. B., Makic, M. B., Martinez-Kratz, M. R., & Zanotti, M. (2020). Nursing diagnoses handbook: An evidence-based guide to planning care. St. Louis, MO: Elsevier. Buy on Amazon
Gulanick, M., & Myers, J. L. (2022). Nursing care plans: Diagnoses, interventions, & outcomes. St. Louis, MO: Elsevier. Buy on Amazon
Ignatavicius, D. D., Workman, M. L., Rebar, C. R., & Heimgartner, N. M. (2018). Medical-surgical nursing: Concepts for interprofessional collaborative care. St. Louis, MO: Elsevier. Buy on Amazon
Silvestri, L. A. (2020). Saunders comprehensive review for the NCLEX-RN examination. St. Louis, MO: Elsevier. Buy on Amazon
Disclaimer:
Please follow your facilities guidelines and policies and procedures.
The medical information on this site is provided as an information resource only and is not to be used or relied on for any diagnostic or treatment purposes.
This information is not intended to be nursing education and should not be used as a substitute for professional diagnosis and treatment.