Edema is the term for swelling caused by excess fluid trapped in the body’s tissues. It commonly affects the extremities, such as the legs, ankles, and feet, but it can occur anywhere in the body.
Edema may be a symptom of various underlying health conditions such as heart failure, kidney disease, liver disease, or even pregnancy.
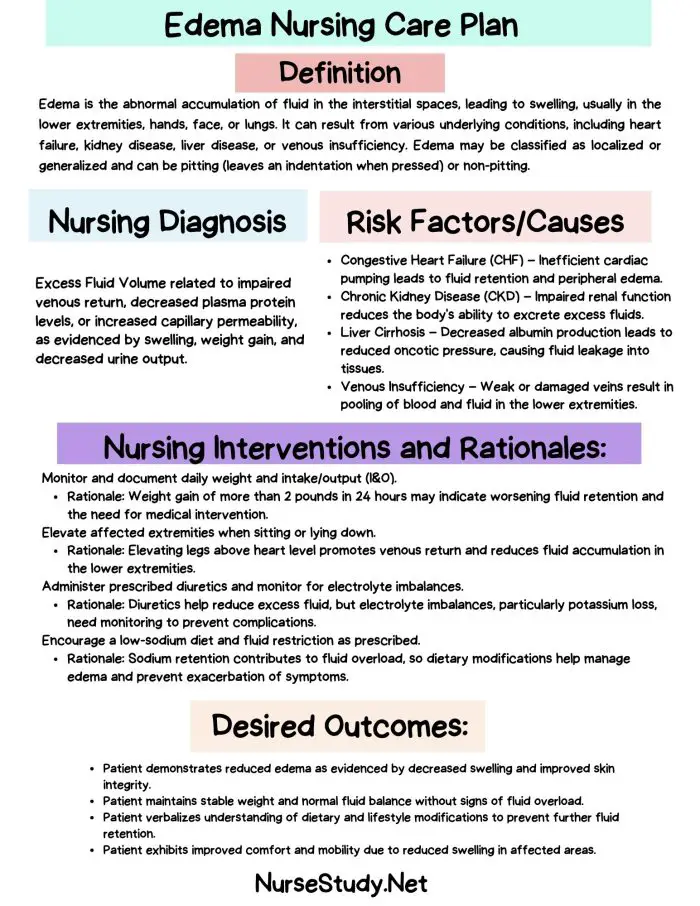
Edema Nursing Diagnosis
Edema occurs when fluid accumulates in the interstitial tissues, leading to swelling. This condition is often due to poor circulation, issues with the lymphatic system, or fluid imbalances caused by heart, liver, or kidney disorders.
Signs and Symptoms:
- Swelling in the affected area
- Stretched or shiny skin over swollen areas
- Pitting (indentation that is left on the skin when pressed)
- Increased abdominal size
- Weight gain
- Shortness of breath (if fluid accumulates in the lungs)
Potential Complications:
- Reduced mobility
- Skin breakdown or ulcers
- Difficulty in performing daily activities
- Increased risk of infection due to skin breakdown
- Decreased tissue perfusion
Nursing Assessment:
A thorough nursing assessment is necessary to identify the cause of edema and monitor its progression. Key assessments include:
- Daily weight monitoring
- Measurement of edema
- Lung auscultation to check for crackles (pulmonary edema)
- Blood pressure monitoring
- Urine output tracking
- Review of laboratory values (serum albumin, electrolytes, and renal function)
Nursing Interventions for Edema
Management of edema requires addressing the underlying cause and implementing nursing care strategies that reduce fluid accumulation.
1. Fluid Restriction and Diuretic Use
In conditions like heart failure or kidney disease, fluid restriction and diuretic medications may be prescribed to decrease fluid retention.
2. Positioning and Elevation
Patients are often encouraged to elevate their legs above heart level to promote venous return and reduce swelling in the lower extremities.
3. Compression Therapy
Compression stockings or wraps are often used to improve circulation and prevent fluid accumulation in the limbs.
4. Skin Care
Proper skin care is essential to prevent breakdown in areas affected by edema. Keep the skin clean, dry, and moisturized.
5. Dietary Management
A low-sodium diet is often recommended to reduce fluid retention. Sodium encourages water retention, which can exacerbate edema.
Edema Nursing Care Plans
Nursing Care Plan 1: Excess Fluid Volume
Nursing Diagnosis Statement: Excess Fluid Volume related to compromised regulatory mechanisms (e.g., heart failure, renal insufficiency) as evidenced by pitting edema, weight gain, and increased blood pressure.
Related Factors/Causes: Heart failure, renal failure, liver disease, excessive sodium intake.
Nursing Interventions and Rationales:
- Monitor daily weight and intake/output.
- Rationale: Sudden weight gain can indicate fluid retention.
- Administer prescribed diuretics (e.g., furosemide).
- Rationale: Diuretics help remove excess fluid and relieve symptoms.
- Encourage the patient to elevate legs above heart level.
- Rationale: Elevation promotes venous return, reducing peripheral edema.
- Implement a low-sodium diet.
- Rationale: Reducing sodium intake decreases fluid retention.
Desired Outcome: The patient will demonstrate decreased edema, as evidenced by weight loss, reduced pitting, and stable blood pressure.
Nursing Care Plan 2: Impaired Skin Integrity
Nursing Diagnosis Statement: Impaired Skin Integrity related to fluid retention and edema as evidenced by pitting edema, shiny and stretched skin, and risk for skin breakdown.
Related Factors/Causes: Peripheral edema, immobility, venous insufficiency.
Nursing Interventions and Rationales:
- Inspect skin regularly for signs of breakdown.
- Rationale: Early identification of skin issues prevents further complications.
- Use mild soap and moisturizer on affected areas.
- Rationale: Keeping the skin clean and moisturized reduces the risk of cracking.
- Apply compression stockings as ordered.
- Rationale: Compression helps improve circulation and prevent fluid buildup.
- Reposition the patient frequently to alleviate pressure.
- Rationale: Frequent repositioning helps prevent pressure ulcers in immobilized patients.
Desired Outcome: The patient will maintain intact skin, free from signs of breakdown or ulceration.
Nursing Care Plan 3: Activity Intolerance
Nursing Diagnosis Statement: Activity Intolerance related to fatigue and shortness of breath secondary to fluid overload as evidenced by inability to tolerate usual activities and dyspnea.
Related Factors/Causes: Heart failure, pulmonary edema, decreased oxygenation.
Nursing Interventions and Rationales:
- Assess the patient’s ability to perform daily activities.
- Rationale: Monitoring helps identify changes in tolerance to activity.
- Plan rest periods between activities.
- Rationale: Rest allows recovery and reduces fatigue.
- Encourage light exercises, such as walking.
- Rationale: Light exercise promotes circulation and reduces edema.
- Monitor oxygen saturation levels during activity.
- Rationale: Oxygen saturation provides an indicator of respiratory function.
Desired Outcome: The patient will demonstrate improved activity tolerance, as evidenced by participation in light activities without dyspnea.
Nursing Care Plan 4: Risk for Infection
Nursing Diagnosis Statement: Risk for Infection related to impaired skin integrity and fluid retention as evidenced by the presence of edema and potential skin breakdown.
Related Factors/Causes: Edematous tissues, poor circulation, and compromised skin integrity.
Nursing Interventions and Rationales:
- Monitor for signs of infection (e.g., redness, warmth, drainage).
- Rationale: Early detection of infection prevents systemic complications.
- Keep skin clean and dry.
- Rationale: Clean, dry skin is less prone to infection.
- Apply prescribed topical antibiotics to any open areas.
- Rationale: Topical antibiotics prevent the spread of bacteria.
- Educate the patient on proper hygiene and skin care.
- Rationale: Patient education promotes adherence to infection prevention practices.
Desired Outcome: The patient will remain free from infection, as evidenced by intact skin and the absence of signs of infection.
Nursing Care Plan 5: Impaired Gas Exchange
Nursing Diagnosis Statement: Impaired Gas Exchange related to fluid overload and pulmonary edema as evidenced by crackles in the lungs, shortness of breath, and low oxygen saturation levels.
Related Factors/Causes: Pulmonary edema, heart failure, fluid overload.
Nursing Interventions and Rationales:
- Assess lung sounds and monitor for crackles.
- Rationale: Crackles indicate fluid in the lungs, which can impair gas exchange.
- Administer supplemental oxygen as prescribed.
- Rationale: Oxygen improves tissue oxygenation and relieves dyspnea.
- Position the patient in a semi-Fowler’s position.
- Rationale: This position allows for better lung expansion and gas exchange.
- Monitor oxygen saturation and respiratory rate.
- Rationale: Monitoring provides an indicator of respiratory status and the effectiveness of interventions.
Desired Outcome: The patient will maintain adequate gas exchange, as evidenced by normal oxygen saturation and clear lung sounds.
References
- Perry, A.G., Potter, P.A., & Ostendorf, W.R. (2018). Clinical Nursing Skills & Techniques. Elsevier.
- McCance, K.L., & Huether, S.E. (2019). Pathophysiology: The Biologic Basis for Disease in Adults and Children. Elsevier.
- Ignatavicius, D.D., & Workman, M.L. (2020). Medical-Surgical Nursing: Patient-Centered Collaborative Care. Elsevier.
- Lewis, S.M., Bucher, L., Heitkemper, M.M., & Harding, M.M. (2020). Medical-Surgical Nursing: Assessment and Management of Clinical Problems. Elsevier.
- Ackley, B.J., & Ladwig, G.B. (2020). Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care. Elsevier.