Cellulitis is a common bacterial skin infection that affects the deeper layers of skin and subcutaneous tissues. This comprehensive guide will explore cellulitis nursing diagnoses, interventions, and care plans to help you provide optimal care for your patients.
What is Cellulitis?
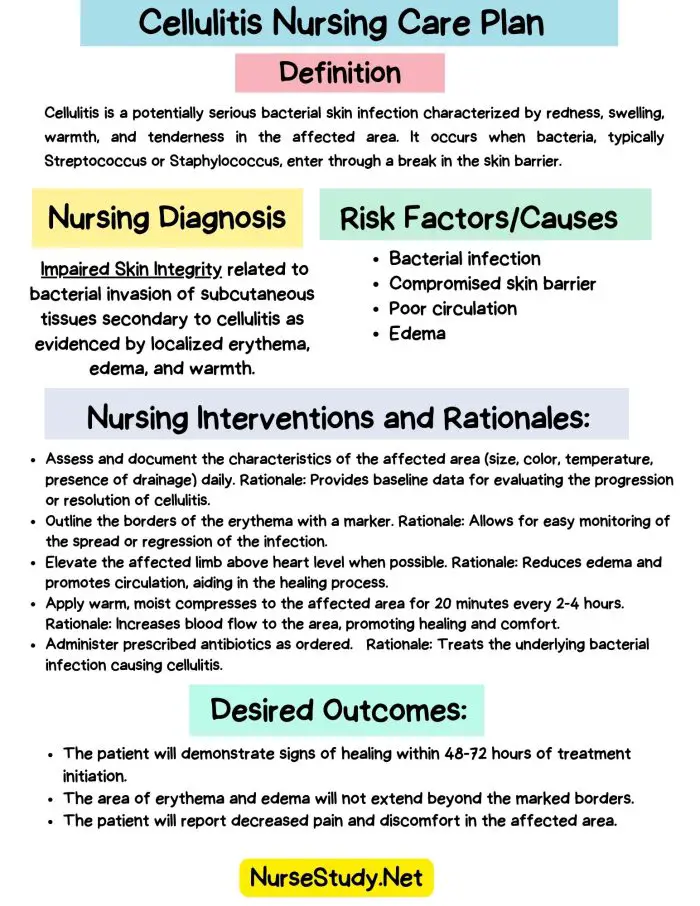
Cellulitis is a potentially serious bacterial skin infection characterized by redness, swelling, warmth, and tenderness in the affected area. It occurs when bacteria, typically Streptococcus or Staphylococcus, enter through a break in the skin barrier.
Common Causes of Cellulitis:
- Cuts, scrapes, or burns
- Insect or animal bites
- Surgical incisions
- Skin conditions like eczema or psoriasis
- Intravenous drug use
- Poor hygiene during tattoos or piercings
Risk Factors:
- Obesity
- Lymphedema
- Diabetes
- Peripheral vascular disease
- Weakened immune system
Cellulitis requires prompt antibiotic treatment to prevent complications such as sepsis, osteomyelitis, or necrotizing fasciitis.
The Nursing Process in Cellulitis Care
As a nurse, your role in caring for patients with cellulitis is crucial. You must assess the patient’s condition, develop appropriate nursing diagnoses, implement interventions, and evaluate outcomes. Education is a crucial component, as patients often need guidance on managing their condition and preventing recurrence.
Cellulitis Nursing Care Plans
Nursing care plans are essential for managing cellulitis. Here are five comprehensive nursing care plans addressing common issues in cellulitis patients:
1. Impaired Skin Integrity
Nursing Diagnosis Statement: Impaired Skin Integrity related to bacterial invasion of subcutaneous tissues secondary to cellulitis as evidenced by localized erythema, edema, and warmth.
Related Factors/Causes:
- Bacterial infection
- Compromised skin barrier
- Poor circulation
- Edema
Nursing Interventions and Rationales:
- Assess and document the characteristics of the affected area (size, color, temperature, presence of drainage) daily.
Rationale: Provides baseline data for evaluating the progression or resolution of cellulitis. - Outline the borders of the erythema with a marker.
Rationale: Allows for easy monitoring of the spread or regression of the infection. - Elevate the affected limb above heart level when possible.
Rationale: Reduces edema and promotes circulation, aiding in the healing process. - Apply warm, moist compresses to the affected area for 20 minutes every 2-4 hours.
Rationale: Increases blood flow to the area, promoting healing and comfort. - Administer prescribed antibiotics as ordered.
Rationale: Treats the underlying bacterial infection causing cellulitis.
Desired Outcomes:
- The patient will demonstrate signs of healing within 48-72 hours of treatment initiation.
- The area of erythema and edema will not extend beyond the marked borders.
- The patient will report decreased pain and discomfort in the affected area.
2. Acute Pain
Nursing Diagnosis Statement: Acute Pain related to inflammatory process of cellulitis as evidenced by patient’s verbal reports of pain, guarding behavior, and facial grimacing.
Related Factors/Causes:
- Tissue inflammation
- Edema
- Pressure on nerve endings
Nursing Interventions and Rationales:
- Assess pain using a standardized pain scale every 4 hours and as needed.
Rationale: Provides objective data for pain management and evaluation of interventions. - Administer prescribed analgesics as ordered.
Rationale: Reduces pain and discomfort associated with cellulitis. - Teach and encourage non-pharmacological pain management techniques (e.g., relaxation, distraction).
Rationale: Complements medication and empowers the patient in pain management. - Position the affected area for comfort, using pillows for support as needed.
Rationale: Reduces pressure on the affected area and promotes comfort. - Monitor for signs of advancing infection (increased pain, fever, malaise).
Rationale: Early detection of complications allows for prompt intervention.
Desired Outcomes:
- The patient will report pain at a level of 3/10 or less within 24 hours of interventions.
- The patient will demonstrate the use of at least one non-pharmacological pain management technique.
- The patient will verbalize understanding of pain management strategies.
3. Risk for Infection (Systemic)
Nursing Diagnosis Statement: Risk for Infection (Systemic) related to localized bacterial infection and potential for spread.
Related Factors/Causes:
- Presence of pathogenic organisms
- Compromised skin integrity
- Chronic health conditions (e.g., diabetes, immunosuppression)
- Delayed or inadequate treatment
Nursing Interventions and Rationales:
- Monitor vital signs, especially temperature, every 4 hours.
Rationale: Fever may indicate spreading infection or sepsis. - Assess the affected area for signs of advancing infection (increased redness, warmth, swelling, purulent drainage) every shift.
Rationale: Early detection of worsening infection allows for prompt intervention. - Obtain blood cultures as ordered before initiating antibiotic therapy.
Rationale: Identifies causative organisms and guides appropriate antibiotic selection. - Ensure proper hand hygiene and use of personal protective equipment.
Rationale: Prevents cross-contamination and protects both patients and healthcare providers. - Educate the patient on the signs and symptoms of worsening infection to report.
Rationale: Enables early detection and prompt treatment of complications.
Desired Outcomes:
- The patient will remain afebrile throughout the hospital stay.
- Patient will show no signs of systemic infection or sepsis.
- The patient will verbalize understanding of signs and symptoms to report.
4. Deficient Knowledge
Nursing Diagnosis Statement: Deficient Knowledge related to lack of familiarity with cellulitis management and prevention as evidenced by the patient’s verbalization of uncertainty and questions about self-care.
Related Factors/Causes:
- Lack of exposure to information
- Misinterpretation of information
- Cognitive limitations
- Language barriers
Nursing Interventions and Rationales:
- Assess the patient’s current understanding of cellulitis, its causes, and management.
Rationale: Identifies knowledge gaps and guides education efforts. - Provide education on cellulitis, including causes, treatment, and prevention strategies.
Rationale: Increases patient’s understanding and promotes self-management skills. - Demonstrate proper wound care and hygiene techniques.
Rationale: Enhances patient’s ability to prevent recurrence and manage the condition. - Discuss the importance of completing the full course of antibiotics.
Rationale: Promotes adherence to treatment and prevents antibiotic resistance. - Provide written materials in the patient’s preferred language.
Rationale: Reinforces verbal education and serves as a reference for the patient.
Desired Outcomes:
- Patient will verbalize understanding of cellulitis, its causes, and prevention strategies.
- The patient will demonstrate proper wound care techniques before discharge.
- Patient will verbalize the importance of completing the full course of antibiotics.
5. Impaired Physical Mobility
Nursing Diagnosis Statement: Impaired Physical Mobility related to pain and edema associated with cellulitis as evidenced by difficulty moving the affected limb and reluctance to ambulate.
Related Factors/Causes:
- Pain in the affected area
- Edema
- Prescribed immobility
- Fear of movement causing pain
Nursing Interventions and Rationales:
- Assess the patient’s level of mobility and limitations every shift.
Rationale: Provides baseline data for planning care and evaluating progress. - Assist with range of motion exercises for unaffected limbs every 4 hours while awake.
Rationale: Maintains joint flexibility and muscle strength, preventing complications of immobility. - Encourage frequent position changes and early ambulation as tolerated.
Rationale: Prevents complications of immobility and promotes circulation. - Provide assistive devices (e.g., walker, cane) as needed.
Rationale: Enhances patient safety and promotes independence in mobility. - Administer prescribed pain medication before activities.
Rationale: Reduces pain and facilitates patient participation in mobility activities.
Desired Outcomes:
- Patient will demonstrate increased mobility within 48 hours of interventions.
- The patient will participate in prescribed mobility exercises with minimal assistance.
- Patient will ambulate safely with appropriate assistive devices as needed.
Conclusion
Effective management of cellulitis requires a comprehensive nursing approach. By implementing these nursing care plans, healthcare professionals can provide optimal care, promote healing, and prevent complications. Remember to tailor these plans to each patient’s unique needs and circumstances.
Continuous assessment, prompt intervention, and patient education are key components in successfully managing cellulitis. Nurses can significantly improve patient outcomes and quality of life by staying informed about best practices in cellulitis care.
References
- Stevens, D. L., & Bryant, A. E. (2016). Cellulitis and Soft Tissue Infections. Annals of Internal Medicine, 164(11), ITC81-ITC96. https://doi.org/10.7326/AITC201606070
- Raff, A. B., & Kroshinsky, D. (2016). Cellulitis: A Review. JAMA, 316(3), 325-337. https://doi.org/10.1001/jama.2016.8825
- Kilburn, S. A., Featherstone, P., Higgins, B., & Brindle, R. (2010). Interventions for cellulitis and erysipelas. Cochrane Database of Systematic Reviews, (6), CD004299. https://doi.org/10.1002/14651858.CD004299.pub2
- Swartz, M. N. (2004). Cellulitis. New England Journal of Medicine, 350(9), 904-912. https://doi.org/10.1056/NEJMcp031807
- Aly, A. A., Roberts, N. M., Seipel, K. S., & MacLellan, R. A. (2017). Case survey of management of cellulitis in a tertiary teaching hospital. Medical Journal of Australia, 206(1), 38-40. https://doi.org/10.5694/mja16.00544
- Hepburn, M. J., Dooley, D. P., Skidmore, P. J., Ellis, M. W., Starnes, W. F., & Hasewinkle, W. C. (2004). Comparison of short-course (5 days) and standard (10 days) treatment for uncomplicated cellulitis. Archives of Internal Medicine, 164(15), 1669-1674. https://doi.org/10.1001/archinte.164.15.1669