Almost everyone experiences acute pain, a highly subjective and unpleasant feeling.
A nursing diagnosis for Acute Pain is defined as an unpleasant emotional and sensory experience resulting from actual or potential damage to body tissue.
It can be sudden or have a slow onset, ranging from mild to severe. The duration can vary from a few seconds to up to six months.
Chronic pain is defined as long-term pain experienced for more than six months.
Signs and Symptoms of Acute Pain
Subjective:
- Complaint of sharp/intense pain
- Throbbing/aching
- Report of difficulty sleeping
- Decreased concentration
- Restlessness
- Anxiety
- Decreased ADL’s
- Dizziness
Objective:
- Increased pulse
- Increased blood pressure
- Facial grimacing
- Guarding the area in pain
- Irritability
- Increased V/S
- Pallor
Related Factors and At-Risk Population
Various factors can cause acute pain, such as:
Pain Assessment Tools
Various pain assessment tools are available for evaluating acute pain, such as the Brief Pain Inventory, Wong-Baker Faces Pain Scale, FLACC, visual analog scale, PQRST pain assessment, numerical rating pain scale, and the Indiana Polyclinic Combined Pain Scale.
Acute Pain Nursing Diagnosis
- Impaired Physical Mobility related to acute pain
- Anxiety related to acute pain
- Disturbed Sleep Pattern related to acute pain
- Ineffective Coping related to acute pain
- Risk for Falls related to acute pain
Expected Outcomes
- Reduction of pain intensity to a manageable level
- Improved ability to perform daily activities
- Enhanced coping strategies for pain management
- Promotion of optimal sleep patterns
- Prevention of complications associated with acute pain
Nursing Interventions for Acute Pain
- Administer pain medications as prescribed. This provides effective acute pain relief to the patient.
- Ask the patient to re-rate his/her acute pain 30 minutes to an hour after administering the analgesic. To assess the effectiveness of treatment and monitor their condition.
- Provide more analgesics at recommended/prescribed intervals. This promotes pain relief and patient comfort without the risk of overdose.
- Reposition the patient in his/her comfortable/preferred position. Repositioning helps relieve pressure on a body part and promotes comfort.
- Encourage pursed lip breathing and deep breathing exercises. This promotes optimal patient comfort and reduces anxiety and restlessness without total dependence on pharmacologic interventions.
- Refer the patient to a pain specialist as required. This enables the patient to receive more information and specialized care if current efforts for pain management are deemed ineffective.
- Explain his/her pain management program (e.g., medications, relaxation techniques, related physiotherapy, or exercises). To provide information on his/her pain management program.
- Inform the patient about each prescribed medication, including drug class, benefits, side effects, and risks. Ask them to demonstrate self-administration details to ensure they understand how to take the medication properly. Explain potential side effects and adverse events, and ensure the patient is aware of associated risks.
- Educate the patient about non-pharmacological methods for acute pain, such as guided imagery, recommended exercises, and relaxation techniques. To reduce stress and to promote optimal pain relief without total dependence on pharmacological means.
- Encourage progressive activity through self-care and exercise as tolerated. Explain the need to reduce sedentary activities such as watching television and using social media over long periods. Alternate periods of physical activity with 60-90 minutes of undisturbed rest. To gradually increase the patient’s tolerance to physical activity and prevent triggering of acute pain by allowing the patient to pace activity versus rest.
Non-Pharmacological Interventions
Non-pharmacological pain relief methods, such as visualization exercises and heat/cold applications, can be employed to augment pain relief efforts.
Additionally, changing positions to relieve pressure and allowing patients ample time to report pain can further enhance pain management outcomes.
Pharmacological Pain Management
When non-pharmacological measures fail to alleviate pain, pain medications become essential in managing acute pain.
Types of pain medication include analgesics and nonsteroidal anti-inflammatory drugs, which can be used to treat mild to moderate pain and are often combined with other pain management techniques for increased effectiveness.
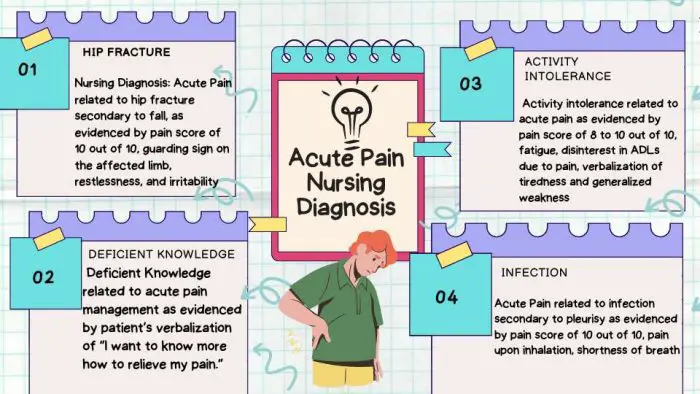
Nursing Care Plans for Acute Pain
Impaired Mobility
Nursing Diagnosis: Impaired Physical Mobility related to acute pain
Related Factors/Causes:
- Acute pain caused by surgical procedure or injury
- Musculoskeletal impairment or dysfunction
- Decreased range of motion due to pain or inflammation
Expected Outcomes:
- The patient will report reduced pain levels within the tolerable range.
- The patient will demonstrate an improved ability to perform mobility-related activities.
- The patient will maintain or regain optimal range of motion.
Nursing Interventions with Rationales:
- Administer prescribed analgesics: Pain management is crucial in promoting mobility, as pain can restrict movement and cause muscle guarding. The nurse helps reduce pain levels by administering analgesics, enabling the patient to engage in mobility exercises effectively.
- Assist the patient with proper positioning and use of assistive devices. Correct positioning helps alleviate pain and ensures comfort during mobility activities. Additionally, assistive devices such as crutches, walkers, or wheelchairs can provide support and stability, promoting safe and effective movement.
- Encourage regular range-of-motion exercises. Range-of-motion exercises help prevent muscle stiffness and joint contractures.
- Provide education on pain management techniques. Teaching the patient about pain management strategies and relaxation exercises can help reduce pain levels and decrease muscle tension.
- Evaluate and reassess the patient’s pain and mobility status frequently. Regular assessment allows the caregivers to monitor the effectiveness of interventions and make any necessary adjustments to the care plan.
Anxiety
Nursing Diagnosis: Anxiety related to acute pain
Related Factors/Causes:
- Fear and uncertainty related to the experience of acute pain.
- Anticipation of pain during medical procedures or interventions.
- Lack of knowledge or understanding about the pain management process.
Expected Outcomes:
- The patient will verbalize reduced anxiety levels and increased feelings of calmness.
- The patient will actively participate in pain management strategies.
- The patient will demonstrate effective coping mechanisms to manage anxiety related to acute pain.
Nursing Interventions with Rationales:
- Provide education & information about pain management. Educating the patient about the nature of acute pain, its causes, and available pain management strategies can help reduce anxiety.
- Encourage the patient to express feelings related to pain & anxiety. Providing a supportive environment for the patient to express emotions can help alleviate anxiety.
- Teach relaxation techniques. This can help manage anxiety by promoting a sense of calmness and reducing physiological arousal.
- Engage the patient in diversional activities. Diversional activities, such as engaging in hobbies, listening to music, or watching movies, can help redirect the patient’s focus away from pain and reduce anxiety.
- Evaluate and reassess the patient’s anxiety levels and coping mechanisms regularly. Regular assessment allows the nurse to monitor the effectiveness of interventions and make any necessary adjustments to the care plan.
Acute Pain Practice NCLEX Questions
Question 1:
A patient presents with acute abdominal pain. The nurse suspects appendicitis. Which assessment finding supports this suspicion?
A) Radiating chest pain
B) Rebound tenderness in the right lower quadrant
C) Bilateral leg swelling
D) Increased urine output
Answer: B) Rebound tenderness in the right lower quadrant
Rationale: Rebound tenderness in the right lower quadrant is a classic sign of appendicitis. It occurs when pressure is applied to the area and then quickly released, resulting in increased pain.
Question 2:
A postoperative patient is experiencing acute pain. Which non-pharmacological intervention would be most effective in providing relief?
A) Administering oral analgesics
B) Applying cold packs to the surgical site
C) Providing distraction with music or games
D) Assisting with relaxation techniques
Answer: D) Assisting with relaxation techniques
Rationale: Non-pharmacological interventions such as relaxation techniques, including deep breathing exercises and guided imagery, can help reduce acute pain and promote relaxation, allowing the patient to experience relief.
Question 3:
A patient with a leg fracture reports severe pain. The nurse understands that pain can lead to which physiological response?
A) Decreased heart rate
B) Increased blood pressure
C) Decreased respiratory rate
D) Decreased oxygen saturation
Answer: B) Increased blood pressure
Rationale: Severe pain activates the sympathetic nervous system, increasing stress hormone release. This response causes vasoconstriction, increasing blood pressure as a compensatory mechanism.
Question 4:
A patient with acute pancreatitis is experiencing severe pain. Which medication is the most appropriate for the nurse to administer?
A) Acetaminophen (Tylenol)
B) Ibuprofen (Advil)
C) Morphine sulfate
D) Aspirin
Answer: C) Morphine sulfate
Rationale: Acute pancreatitis is a severe and painful condition. Morphine sulfate, an opioid analgesic, is the most appropriate medication to relieve severe pain in this situation.
Question 5:
A patient with acute respiratory distress syndrome (ARDS) is experiencing severe pain due to rib fractures. Which nursing intervention should take priority?
A) Administering supplemental oxygen
B) Applying ice packs to the fractured ribs
C) Administering intravenous fluids
D) Providing distraction with music or games
Answer: A) Administering supplemental oxygen
Rationale: In a patient with ARDS, maintaining adequate oxygenation is crucial. Administering supplemental oxygen takes priority as it helps meet the patient’s respiratory needs and promotes adequate oxygen saturation, supporting healing and alleviating pain associated with rib fractures.
Nursing References
Ackley, B. J., Ladwig, G. B., Makic, M. B., Martinez-Kratz, M. R., & Zanotti, M. (2020). Nursing diagnoses handbook: An evidence-based guide to planning care. St. Louis, MO: Elsevier.
Gulanick, M., & Myers, J. L. (2017). Nursing care plans: Diagnoses, interventions, & outcomes. St. Louis, MO: Elsevier.
Hyland SJ, Wetshtein AM, Grable SJ, Jackson MP. Acute Pain Management Pearls: A Focused Review for the Hospital Clinician. Healthcare. 2023; 11(1):34. https://doi.org/10.3390/healthcare11010034
Ignatavicius, D. D., Workman, M. L., Rebar, C. R., & Heimgartner, N. M. (2018). Medical-surgical nursing: Concepts for interprofessional collaborative care. St. Louis, MO: Elsevier.
Johnson, Q., Borsheski, R. R., & Reeves-Viets, J. L. (2013). Pain management mini-series. Part I. A review of management of acute pain. Missouri medicine, 110(1), 74–79.
Silvestri, L. A. (2020). Saunders comprehensive review for the NCLEX-RN examination. St. Louis, MO: Elsevier.
Wardhan, R., & Chelly, J. (2017). Recent advances in acute pain management: understanding the mechanisms of acute pain, the prescription of opioids, and the role of multimodal pain therapy. F1000Research, 6, 2065. https://doi.org/10.12688/f1000research.12286.1
Disclaimer:
Please follow your facility’s guidelines policies, and procedures.
The medical information on this site is provided as an information resource and is not to be used or relied on for diagnostic or treatment purposes.
This information is not intended to be nursing education and should not be used as a substitute for professional diagnosis and treatment.
Best Nursing Books and Resources
These are the nursing books and resources that we recommend.
NurseStudy.net is a participant in the Amazon Services LLC Associates Program. Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. Please see our Privacy Policy

The Nursing Diagnosis Handbook E-Book: An Evidence-Based Guide to Planning Care
This is an excellent reference for nurses and nursing students. While it is a great resource for writing nursing care plans and nursing diagnoses, it also helps guide the nurse to match the nursing diagnosis to the patient assessment and diagnosis.
This handbook has been updated with NANDA-I approved Nursing Diagnoses that incorporates NOC and NIC taxonomies and evidenced based nursing interventions and much more.
NANDA International Nursing Diagnoses: Definitions & Classification, 2021-2023
All introductory chapters in this updated version of a ground-breaking text have been completely rewritten to give nurses the knowledge they require to appreciate assessment, its relationship to diagnosis and clinical reasoning, and the goal and use of taxonomic organization at the bedside.
Nursing Care Plans: Nursing Diagnosis and Intervention
It contains more than 200 care plans that adhere to the newest evidence-based recommendations.
Additionally, it distinguishes between nursing and collaborative approaches and highlights QSEN competencies.


