Definition of GI Bleed:
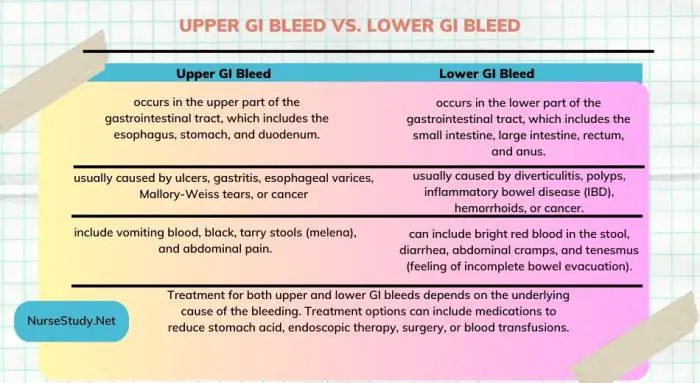
GI Bleed refers to the loss of blood from the gastrointestinal tract, which includes the esophagus, stomach, small intestine, or large intestine. This condition can range from minor, self-limiting bleeding to severe, life-threatening hemorrhage.
Defining Characteristics of GI Bleed:
Subjective:
- Complaints of abdominal pain or discomfort
- Feeling lightheaded or dizzy
- History of recent gastrointestinal surgery or procedures
- Reports of previous episodes of GI bleeding
Objective:
- Presence of blood in vomit (hematemesis)
- Blood in the stool (melena or hematochezia)
- Drop in blood pressure and tachycardia
- Pallor or signs of anemia
- Signs of hypovolemia such as thirst, decreased urine output, and cool clammy skin
- Positive guaiac test indicating the presence of occult blood in the stool
Related Factors:
- Peptic ulcers
- Gastritis or esophagitis
- Gastrointestinal malignancies
- Diverticular disease
- Esophageal varices
- Coagulation disorders
- Medication use (such as non-steroidal anti-inflammatory drugs or anticoagulants)
- Trauma or injury to the gastrointestinal tract
Risk Population: Individuals at higher risk for GI bleeding include:
- Older adults
- Individuals with a history of gastrointestinal diseases or surgeries
- Patients taking medications that increase the risk of bleeding
- Individuals with coagulation disorders
- Those with a history of alcohol abuse
Associated Problems:
- Anemia
- Hypovolemia
- Hypotension
- Fluid and electrolyte imbalances
- Impaired tissue perfusion
- Acute pain
Suggestions for Use:
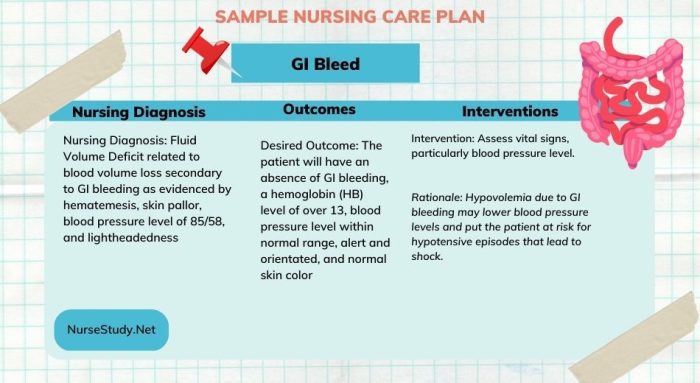
The nursing diagnosis of GI Bleed should be considered when a patient presents with signs and symptoms indicative of gastrointestinal bleeding. It is essential to assess the individual thoroughly and gather relevant subjective and objective data to support the diagnosis. Prompt medical intervention is crucial in managing this condition.
Suggested Alternative NANDA Diagnoses:
These will will formulate a GI bleed nursing care plan.
- Risk for Deficient Fluid Volume
- Risk for Ineffective Tissue Perfusion
- Acute Pain
- Risk for Electrolyte Imbalance
- Risk for Impaired Gas Exchange
Usage Tips:
- Assess vital signs frequently and monitor for signs of bleeding, such as hematemesis or melena.
- Monitor laboratory values, including hemoglobin and hematocrit levels, coagulation studies, and blood typing and cross-matching.
- Encourage the patient to report any changes in pain, dizziness, or the presence of blood in the stool or vomit.
- Collaborate with the healthcare team to ensure appropriate diagnostic tests, interventions, and treatments are implemented.
NOC Outcomes:
- Tissue Perfusion: Cardiopulmonary
- Fluid Balance
- Hemodynamic Control
- Pain Level
- Knowledge: Medication Management
- Knowledge: Treatment Regimen
NOC Results:
The expected outcomes may vary based on the severity of the GI bleed and the patient’s overall health. Desired results include stable hemodynamic status, adequate tissue perfusion, restoration of fluid balance, relief of pain, understanding of medication management, and adherence to the treatment regimen.
NIC Interventions:
Nursing Interventions for GI Bleed.
- Monitor Vital Signs
- Assess Bleeding and Hemodynamic Status
- Administer Intravenous Fluids and Blood Products as Prescribed
- Administer Medications as Prescribed (e.g., Proton Pump Inhibitors, Antiemetics, Hemostatic Agents)
- Provide Patient and Family Education
- Facilitate Endoscopic Interventions or Surgical Consultation as Indicated
- Monitor and Manage Potential Complications (e.g., Anemia, Hypovolemia, Electrolyte Imbalances)
- Collaborate with the Interdisciplinary Team for Blood Transfusions or Coagulation Support
- Provide Emotional Support and Education to the Patient and Family
- Promote Safety Measures and Fall Prevention
Nursing Test Questions for GI Bleed
Question 1: A patient with a history of peptic ulcers is admitted to the hospital with signs and symptoms of gastrointestinal bleeding. Which nursing diagnosis is most appropriate for this patient?
a) Risk for Impaired Gas Exchange
b) Ineffective Tissue Perfusion
c) Risk for Deficient Fluid Volume
d) Acute Pain
Answer: c) Risk for Deficient Fluid Volume
Rationale: The patient with gastrointestinal bleeding is at risk for deficient fluid volume due to ongoing blood loss. This nursing diagnosis focuses on the potential complication of decreased circulating blood volume.
Question 2: Which of the following is a defining characteristic of GI bleeding?
a) Fever
b) Cyanosis
c) Black, tarry stools (melena)
d) Abdominal distension
Answer: c) Black, tarry stools (melena)
Rationale: Melena, which refers to black, tarry stools, is a characteristic sign of gastrointestinal bleeding and suggests the presence of blood in the upper gastrointestinal tract.
Question 3: A patient with GI bleeding is experiencing hypotension and tachycardia. Which intervention should the nurse prioritize?
a) Administering pain medication
b) Providing emotional support
c) Assessing for signs of ongoing bleeding
d) Assisting with ambulation
Answer: c) Assessing for signs of ongoing bleeding
Rationale: The priority intervention is to assess for signs of ongoing bleeding to determine the extent of the hemorrhage and intervene promptly. Hypotension and tachycardia may indicate significant blood loss.
Question 4: Which related factor increases the risk of GI bleeding?
a) Regular exercise
b) Chronic alcohol abuse
c) Adequate fluid intake
d) High-fiber diet
Answer: b) Chronic alcohol abuse
Rationale: Chronic alcohol abuse can contribute to the development of gastrointestinal ulcers and increased susceptibility to GI bleeding.
Question 5: The nurse is caring for a patient with suspected GI bleeding. Which laboratory test is most important to assess the patient’s blood loss?
a) Complete blood count (CBC)
b) Electrocardiogram (ECG)
c) Urinalysis d) Blood glucose level
Answer: a) Complete blood count (CBC)
Rationale: The CBC provides essential information about the patient’s hemoglobin and hematocrit levels, which can indicate the extent of blood loss and the need for further interventions such as blood transfusions.
Nursing References
Ackley, B. J., Ladwig, G. B., Makic, M. B., Martinez-Kratz, M. R., & Zanotti, M. (2020). Nursing diagnoses handbook: An evidence-based guide to planning care. St. Louis, MO: Elsevier.
Gulanick, M., & Myers, J. L. (2022). Nursing care plans: Diagnoses, interventions, & outcomes. St. Louis, MO: Elsevier.
Ignatavicius, D. D., Workman, M. L., Rebar, C. R., & Heimgartner, N. M. (2018). Medical-surgical nursing: Concepts for interprofessional collaborative care. St. Louis, MO: Elsevier.
Silvestri, L. A. (2020). Saunders comprehensive review for the NCLEX-RN examination. St. Louis, MO: Elsevier.
Best Nursing Books and Resources
These are the nursing books and resources that we recommend.
NurseStudy.net is a participant in the Amazon Services LLC Associates Program. Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. Please see our Privacy Policy

The Nursing Diagnosis Handbook E-Book: An Evidence-Based Guide to Planning Care
This is an excellent reference for nurses and nursing students. While it is a great resource for writing nursing care plans and nursing diagnoses, it also helps guide the nurse to match the nursing diagnosis to the patient assessment and diagnosis.
This handbook has been updated with NANDA-I approved Nursing Diagnoses that incorporates NOC and NIC taxonomies and evidenced based nursing interventions and much more.
NANDA International Nursing Diagnoses: Definitions & Classification, 2021-2023
All introductory chapters in this updated version of a ground-breaking text have been completely rewritten to give nurses the knowledge they require to appreciate assessment, its relationship to diagnosis and clinical reasoning, and the goal and use of taxonomic organization at the bedside.
Nursing Care Plans: Nursing Diagnosis and Intervention
It contains more than 200 care plans that adhere to the newest evidence-based recommendations.
Additionally, it distinguishes between nursing and collaborative approaches and highlights QSEN competencies.
Disclaimer:
Please follow your facilities guidelines and policies and procedures. The medical information on this site is provided as an information resource only and is not to be used or relied on for any diagnostic or treatment purposes. This information is not intended to be nursing education and should not be used as a substitute for professional diagnosis and treatment.



i find it so helpful that i wanted to subscribe but i did not because i did not find the subscribe option…I appreciate
Very detailed and informative