Disuse syndrome is a condition that affects individuals who experience decreased use of body parts or movement. This condition can lead to impaired functioning and may compromise health.
The nursing diagnosis of risk for disuse syndrome is classified within the domain of altered health maintenance. It is defined as a state in which an individual is at risk for impaired functioning due to decreased use of body parts or movement.
Patients who are bedridden or have limited mobility due to illness or injury are at high risk for developing disuse syndrome.
Nurses must carefully assess patients for signs of disuse syndrome, such as muscle weakness, joint stiffness, pain, and decreased range of motion. They must also work with other healthcare professionals to develop appropriate interventions to prevent the onset of this condition.
By identifying patients who are at risk for disuse syndrome and developing appropriate care plans, nurses can help to improve patient outcomes and prevent complications associated with this condition.
Understanding Risk for Disuse Syndrome Nursing Diagnosis
Definition
Disuse syndrome nursing diagnosis is a clinical judgment made by a nurse to identify an individual at risk for developing disuse syndrome. Disuse syndrome is a condition that occurs due to prolonged immobility, leading to physical deconditioning, muscle atrophy, and decreased functional ability.
The nursing diagnosis is based on the NANDA-I classification system and is used to guide the development of a nursing care plan.
Causes
Disuse syndrome can be caused by a variety of factors, including injury, illness, or prolonged bed rest. When an individual is immobile, their muscles become weak, and their bones lose density.
This can lead to a decreased range of motion, decreased strength, and increased risk of falls. Disuse syndrome can also lead to other complications such as pressure ulcers, pneumonia, and urinary tract infections.
Risk Factors
Some of the risk factors associated with hospitalized patients with disuse syndrome include prolonged bed rest, impaired physical mobility due to injury or illness, and decreased physical activity.
Other risk factors may include fatigue, fear of injury, and decreased self-care abilities. Nurses must assess these risk factors and develop a nursing care plan that addresses the individual’s specific needs.
In conclusion, the risk for disuse syndrome nursing diagnosis is an essential tool for nurses to identify individuals at risk of developing disuse syndrome.
By understanding the causes and risk factors associated with this condition, nurses can develop an effective nursing care plan that promotes movement, prevents injury, and improves overall health outcomes.
Assessment and Diagnosis of Risk for Disuse Syndrome
Nursing Assessment
To assess the risk for disuse syndrome, the nurse should evaluate the patient’s level of physical activity, mobility, and ability to perform daily activities. The nurse should also assess the patient’s medical history, including any chronic illnesses, trauma, surgery, or medication use that may increase the risk for disuse syndrome.
Additionally, the nurse should assess the patient’s risk factors for developing disuse syndrome, such as age, obesity, and smoking history.
During the assessment, the nurse should also evaluate the patient’s body systems, including the musculoskeletal, cardiovascular, respiratory, and gastrointestinal systems, for signs of deterioration.
The nurse should also assess the patient’s family and social support system to determine if there are any barriers to physical activity or mobility.
Nursing Diagnosis
The nursing diagnosis for risk for disuse syndrome is “At risk of deterioration of body systems as the result of prescribed or unavoidable musculoskeletal inactivity” (NANDA-I). This diagnosis represents a collection of nursing diagnoses that usually occur together, including pressure ulcer, constipation, pulmonary stasis, thrombosis, and body image disturbance.
To make a nursing diagnosis of risk for disuse syndrome, the nurse should consider the patient’s risk factors, medical history, and physical assessment findings. The nurse should also consider the patient’s goals and preferences when developing a plan of care.
Nursing Interventions
Nursing interventions for risk for disuse syndrome should focus on promoting physical activity, mobility, and independence. The nurse should encourage the patient to participate in physical therapy, range of motion exercises, and activities of daily living as appropriate. The nurse should also promote safety by assessing the patient’s risk for falls and implementing fall prevention measures.
To prevent deterioration of body systems, the nurse should implement interventions to prevent pressure ulcers, constipation, pulmonary stasis, and thrombosis.
The nurse should also address any body image disturbances by providing emotional support and education about the effects of inactivity on the body.
Nursing interventions should focus on promoting physical activity, mobility, and independence while preventing deterioration of body systems and addressing any body image disturbances.
Complications of Risk for Disuse Syndrome
Individuals who are at risk for disuse syndrome are at risk of developing complications as a result of prolonged bed rest or physical inactivity.
These complications can have a significant impact on the individual’s overall health and well-being.
Muscle Atrophy
This is a common complication associated with prolonged bed rest or physical inactivity. It is characterized by a decrease in muscle mass and strength. Individuals who are at risk for disuse syndrome are at a higher risk of developing muscle atrophy due to the lack of physical activity. Muscle atrophy can lead to weakness, decreased mobility, and an increased risk of falls and injuries.
Weakness
Weakness is another common complication associated with the risk for disuse syndrome. It is characterized by a decrease in muscle control and strength and can be caused by prolonged bed rest or physical inactivity.
Weakness can lead to impaired physical mobility, activity intolerance, and an increased risk of falls and injuries.
Depression and Anxiety
Prolonged bed rest or physical inactivity can also lead to depression and anxiety. Individuals who are at risk for disuse syndrome may experience feelings of helplessness, loss of control, and social isolation. Depression and anxiety can have a significant impact on an individual’s overall health and well-being.
Physical Activity and Mobility
Physical activity and mobility can also be affected by the risk for disuse syndrome. Individuals who are at risk may experience impaired physical mobility, activity intolerance, and an increased risk of falls and injuries.
It is important for individuals who are at risk for disuse syndrome to engage in physical activity as much as possible to maintain their physical function and mobility.
Constipation
Constipation is another complication associated with the risk for disuse syndrome. It is characterized by infrequent bowel movements and can be caused by prolonged bed rest or physical inactivity. Constipation can lead to discomfort, pain, and other health problems.
Sexual Dysfunction
Sexual dysfunction can also be a complication associated with the risk for disuse syndrome. It is characterized by a decrease in sexual desire or function and can be caused by prolonged bed rest or physical inactivity.
Sexual dysfunction can have a significant impact on an individual’s overall quality of life.
Management and Treatment of Risk for Disuse Syndrome
Goals of Treatment
The primary goal of treatment for risk for disuse syndrome is to prevent the patient from experiencing any complications associated with physical inactivity.
This includes maintaining muscle strength, preventing contractures, and improving coordination. Additionally, treatment should aim to improve the patient’s ability to perform activities of daily living and bed mobility.
Nursing Interventions
Nursing interventions for risk for disuse syndrome include frequent turning and repositioning of the patient to prevent pressure ulcers, encouraging the patient to perform range of motion exercises, and providing assistance with activities of daily living.
Communication is also important in nursing interventions. Nurses should regularly communicate with the patient to ensure that they are comfortable and to assess their level of pain.
Additionally, nurses should educate the patient on the importance of physical activity and encourage them to participate in exercise therapy.
Pharmacologic Support
Pharmacologic support may be necessary to manage symptoms associated with risk for disuse syndrome. For example, patients who experience severe pain may require pain medication. Patients who have difficulty sleeping may require medications to manage insomnia.
Physical and Occupational Therapy
Physical and occupational therapy can be helpful in managing risk for disuse syndrome. These therapies aim to improve the patient’s ability to perform activities of daily living and bed mobility. Additionally, physical therapy can help to maintain muscle strength and prevent contractures.
Counseling and Emotional Support
Patients who are at risk for disuse syndrome may experience feelings of hopelessness or depression. Counseling and emotional support can be helpful in managing these feelings. Additionally, counseling can help patients to develop coping strategies and improve their self-care deficit.
Overall, the management and treatment of risk for disuse syndrome requires a comprehensive approach that addresses the patient’s physical, emotional, and psychological needs.
Nurses should regularly assess the patient’s nutritional status, vital signs, and skin integrity to ensure that they are receiving appropriate care.
Additionally, nurses should work closely with physical and occupational therapists to develop a management guide that is tailored to the patient’s individual needs.
Risk for Disuse Syndrome Nursing Care Plans
Nursing Diagnosis: Risk for Disuse Syndrome
Related Factors:
- Immobility due to illness, injury, or bed rest.
- Limited mobility or physical activity restrictions.
- Prolonged periods of sedentary behavior.
- Musculoskeletal impairment or weakness.
- Neurological conditions affecting mobility.
Expected Outcomes:
- The patient will maintain or regain optimal physical function.
- The patient will demonstrate improved mobility and muscle strength.
- The patient will have a reduced risk of developing complications related to disuse syndrome.
- The patient will participate in therapeutic exercises and activities as appropriate.
- The patient will demonstrate understanding of the importance of maintaining mobility and engaging in regular physical activity.
- The patient will be able to perform exercises independently.
Nursing Assessments with Rationales:
- Assess the patient’s mobility status, including the ability to perform activities of daily living (ADLs) and range of motion (ROM). Rationale: It helps identify the patient’s baseline functional abilities and any limitations or impairments that may contribute to the risk of disuse syndrome.
- Assess the patient’s pain level and provide appropriate pain management interventions. Rationale: Pain can be a barrier to physical activity and mobility, leading to disuse syndrome.
- Assess the patient’s psychological and emotional well-being. Rationale: Psychological factors such as depression, anxiety, or fear can impact motivation and willingness to engage in physical activity, increasing the risk of disuse syndrome.
- Assess the patient’s nutritional status and ensure an adequate intake of nutrients necessary for maintaining muscle strength and bone health. Rationale: Proper nutrition plays a vital role in preventing muscle wasting and promoting overall physical health.
- Assess the patient’s knowledge and understanding of the importance of regular physical activity and the risks associated with prolonged immobility. Rationale: Identifying knowledge gaps helps tailor patient education and promote informed decision-making regarding mobility and physical activity.
Nursing Interventions with Rationales:
- Collaborate with the healthcare team to develop an individualized plan of care focused on improving mobility and preventing disuse syndrome. Rationale: A multidisciplinary approach ensures comprehensive care and addresses the patient’s specific needs and goals.
- Encourage and assist the patient in performing appropriate exercises and activities within their physical capabilities. Rationale: Regular exercise and activity help maintain muscle strength, joint flexibility, and overall physical function, reducing the risk of disuse syndrome.
- Promote a safe environment for mobility, considering the patient’s limitations and any assistive devices required. Rationale: Creating a safe environment encourages the patient to engage in physical activity without fear of falls or injuries.
- Provide education to the patient and their family/caregivers about the importance of regular physical activity and techniques for maintaining mobility during periods of limited activity. Rationale: Education empowers the patient and their support system to actively participate in preventing disuse syndrome.
- Collaborate with the physical or occupational therapist to develop a progressive mobility program tailored to the patient’s abilities and goals. Rationale: Working with specialists ensures the implementation of evidence-based interventions and maximizes the patient’s potential for functional improvement.
Other Nanda Nursing Diagnosis
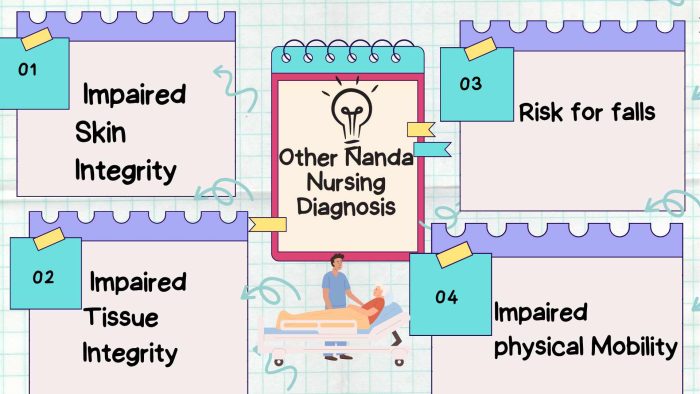
- Impaired physical mobility
- Risk for falls
- Impaired skin integrity
- Impaired tissue integrity
- Risk for injury
Frequently Asked Questions
What is disuse syndrome?
Disuse syndrome is a condition that occurs when an individual is immobile for a long period of time. This can happen due to a variety of reasons, such as being bedridden, hospitalized, or sedentary.
Disuse syndrome can lead to a variety of complications, such as muscle atrophy, joint pain, decreased bone density, skin breakdown, and decreased cardiovascular function.
What are the risk factors for disuse syndrome?
The risk factors for disuse syndrome include prolonged immobility, advanced age, chronic illness, and injury.
Patients who are bedridden or confined to a wheelchair for a long period of time are also at risk for disuse syndrome.
What are the symptoms of disuse syndrome?
The symptoms of disuse syndrome can vary depending on the severity of the condition. Some common symptoms include muscle weakness, decreased range of motion, decreased endurance, decreased bone density, and decreased cardiovascular function.
How can disuse syndrome be prevented?
Disuse syndrome can be prevented by encouraging patients to stay active and mobile, even if they are bedridden or confined to a wheelchair. This can be achieved through exercises that target the affected muscles, such as range of motion exercises, resistance training, and cardiovascular exercises.
What is the nursing care plan for long-term bedridden patients?
The nursing care plan for long-term bedridden patients includes a variety of interventions to prevent disuse syndrome. These interventions may include range of motion exercises, resistance training, and cardiovascular exercises. The nursing care plan may also include measures to prevent pressure ulcers, such as turning and repositioning the patient regularly.
What are some interventions for patients at risk for disuse syndrome?
Interventions for patients at risk for disuse syndrome may include range of motion exercises, resistance training, and cardiovascular exercises. Other interventions may include measures to prevent pressure ulcers, such as turning and repositioning the patient regularly, and providing adequate nutrition and hydration.
References
Ackley, B. J., Ladwig, G. B., Makic, M. B., Martinez-Kratz, M. R., & Zanotti, M. (2020). Nursing diagnoses handbook: An evidence-based guide to planning care. St. Louis, MO: Elsevier.
Bortz WM 2nd. The disuse syndrome. West J Med. 1984 Nov;141(5):691-4. PMID: 6516349; PMCID: PMC1011199.
Gulanick, M., & Myers, J. L. (2022). Nursing care plans: Diagnoses, interventions, & outcomes. St. Louis, MO: Elsevier.
Ignatavicius, D. D., Workman, M. L., Rebar, C. R., & Heimgartner, N. M. (2020). Medical-surgical nursing: Concepts for interprofessional collaborative care. St. Louis, MO: Elsevier.
Silvestri, L. A. (2020). Saunders comprehensive review for the NCLEX-RN examination. St. Louis, MO: Elsevier.
Trudel J, deWolfe VG, Young JR, LeFevre FA. Disuse Phenomenon of Lower Extremity: Diagnosis and Treatment. JAMA. 1963;186(13):1129–1131. doi:10.1001/jama.1963.03710130025007
Best Nursing Books and Resources
These are the nursing books and resources that we recommend.
NurseStudy.net is a participant in the Amazon Services LLC Associates Program. Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. Please see our Privacy Policy

The Nursing Diagnosis Handbook E-Book: An Evidence-Based Guide to Planning Care
This is an excellent reference for nurses and nursing students. While it is a great resource for writing nursing care plans and nursing diagnoses, it also helps guide the nurse to match the nursing diagnosis to the patient assessment and diagnosis.
This handbook has been updated with NANDA-I approved Nursing Diagnoses that incorporates NOC and NIC taxonomies and evidenced based nursing interventions and much more.
NANDA International Nursing Diagnoses: Definitions & Classification, 2021-2023
All introductory chapters in this updated version of a ground-breaking text have been completely rewritten to give nurses the knowledge they require to appreciate assessment, its relationship to diagnosis and clinical reasoning, and the goal and use of taxonomic organization at the bedside.
Nursing Care Plans: Nursing Diagnosis and Intervention
It contains more than 200 care plans that adhere to the newest evidence-based recommendations.
Additionally, it distinguishes between nursing and collaborative approaches and highlights QSEN competencies.
Disclaimer
Please follow your facility’s guidelines, policies, and procedures.
The medical information on this site is provided as an information resource only and is not to be used or relied on for diagnostic or treatment purposes.
This information is intended to be nursing education and should not be used as a substitute for professional diagnosis and treatment.


