Last updated on May 4th, 2023 at 02:50 pm
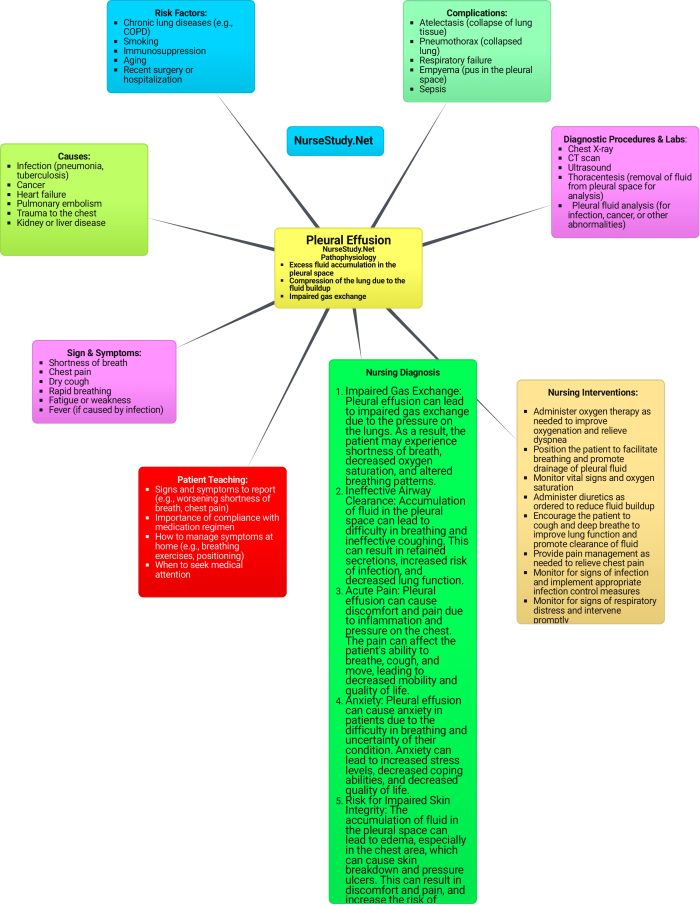
An unusual increase in the fluid in the pleural space will result to a condition called pleural effusion.
Pleural effusion, if left untreated, will hinder with normal respiration and thus, could be life threatening. Some of the signs and symptoms seen in these patients include: shortness of breath, chest pain or chest tightness, dry cough, fatigue, and fever.
Some of the most common causes include: pulmonary embolism, cancer, CHF, pneumonia, autoimmune disease, and TB.
Diagnosis can be made by:
- Chest X-Ray
- CT
- Ultrasound
Patient Teaching & Education
- Understanding of Pleural Effusion
- Report worsening signs and symptoms
- Teach importance of medication compliance
- Lifestyle changes
- Attend all follow up appointments
Nursing Care Plans for Pleural Effusion
Acute Pain
Acute pain happens in pleural effusion because of the excess fluid pushing up against the nerve ending on chest cavity.
Nursing Diagnosis: Acute Pain
Related to:
- Inflammation
- Increased Fluid
- Irritation
As Evidenced By:
- Chest pain
- Facial grimacing
- An elevation in vital signs
Expected Outcomes:
- The patient will report a pain reduction of 2 or 3 on pain scale.
- The patient will be able to participate in ADL’s easily without experiencing increased levels of pain.
Nursing Assessment with Rationales:
- Assess the patient’s level of pain. This helps to identify the source of the pain, and will help to determine the approriate intenventions.
- Assess patient vital signs. This helps identify physiological changes due to pain.
- Determine the patient’s current response to pain management: This will help the health care providers determine if changes need to by made to the current plan.
Nursing Interventions and Rationales:
- Assess the patient using a 0-10 pain rating scale for intensity, as well as characteristics and location of pain (sharp, dull, crushing, etc.). To assist in creating an accurate diagnosis and treating the underlying cause of pain.
- Administer the prescribed pain medications and assess response at least 30 minutes after drug administration. To alleviate the pain and to monitor the efficacy of pharmacological pain relief.
- Educate patient on deep breathing exercises and relaxation techniques. Deep breathing exercises help reduce the incidence of ineffective shallow breathing which is common a response of a patient who has pleuritic pain. Relaxation techniques relieves stress and lowers energy demands.
- Assist the patient to change positions as tolerated. Encourage the patient to lie on the affected side if possible. According to Gate Control Theory of Pain, non-painful sensations such as putting pressure by lying on the affected side can reduce pain perception.
Ineffective Breathing Pattern
Ineffective Breathing Pattern occurs due to the increased pain that the patient experiences.
Nursing Diagnosis: Ineffective Breathing Pattern
Related to:
- Inflammation in the pleura
- Increased Fluid in the pleura
As Evidenced By:
- Dyspnea
- Tachypnea
- Decreased O2 Sats
Expected Outcomes:
- The patient will have a decrease in need for supplemental O2
- The patient will report decreased SOB
- The patient will be able to participate in ADL’s without fatigue.
Nursing Assessment with Rationales:
- Assess the patient’s respirations. Include depth and pattern. The will help monitor the patient’s respiratory status.
- Assess the patient’s need of supplemental O2. This will help monitor if changes need to be made to the plan of care.
Nursing Interventions and Rationales:
- Assess the patient’s vital signs and characteristics of respirations at least every 4 hours. To assist in creating an accurate diagnosis and monitor effectiveness of medical treatment.
- Administer the prescribed antibiotic medications. To treat bacterial infection if this is the underlying cause of the patient’s pleural effusion.
- Administer oxygen therapy as prescribed. To improve oxygenation in the body, aiming for a target level of oxygen saturation (usually above 96%).
- Elevate the head of the bed. Head elevation helps improve the expansion of the lungs, enabling the patient to breathe more effectively.
- Prepare the patient for surgery, as ordered. Pleural effusion can be resolved by putting a pleural drain, performing pleurodesis, VATS, or thoracotomy.
Activity Intolerance
Activity Intolerance occurs due to the patient’s increased level of pain and dyspnea.
Nursing Diagnosis: Activity intolerance
Related to:
- Decreased lung function
- Decreased O2 sat
As Evidenced By:
- Fatigue
- SOB with exertion
- Decreased mobility
- Decreased activity tolerance
Expected Outcomes:
- The patient will be able to do ADL’s without fatigue
- The patient will be able to participate in activities without SOB
Nursing Assessment with Rationales:
- Assess the patient’s current activity levels. The will help to identify the patient’s limitations and abilities.
- Assess the patient’s respiratory status. This will help the health care team identify any physiological changes.
- Assess the current response to ADL’s and acitivity programs. This will help the healthcare team determine if changes need to be made to the current plan of care.
- Assess patient coping stategies. This will help the team determine if the patient needs assistance to improve the quality of life.
Nursing Interventions and Rationales:
- Assess the patient’s activities of daily living, as well as actual and perceived limitations to physical activity. Ask for any form of exercise that he/she used to do or wants to try. To create a baseline of activity levels and mental status related to acute pain, fatigue and activity intolerance.
- Encourage progressive activity through self-care and exercise as tolerated. Explain the need to reduce sedentary activities such as watching television and using social media in long periods. Alternate periods of physical activity with 60-90 minutes of undisturbed rest. To gradually increase the patient’s tolerance to physical activity. To prevent triggering of acute pain by allowing the patient to pace activity versus rest.
- Administer analgesics as prescribed prior to exercise/ physical activity. Teach deep breathing exercises and relaxation techniques. Provide adequate ventilation in the room. To provide pain relief before an exercise session. To allow the patient to relax while at rest and to facilitate effective stress management. To allow enough oxygenation in the room.
- Refer the patient to physiotherapy / occupational therapy team as required. To provide a more specialized care for the patient in terms of helping him/ her build confidence in increasing daily physical activity.
Impaired Gas Exchange
Impaired Gas Exchange occurs when the increase in fluid from the pleural space compresses the lungs and results in decreased oxygen saturations.
Nursing Diagnosis: Impaired Gas Exchange
Related To:
- Excess fluid in pleural space
- decreased lung expansion
As Evidenced By:
- Dyspnea
- Decreased O2 saturations
- Tachypnea
- Abnormal ABG’s
Expected Outcomes:
- The patient will display improved gas exchange
- The patient will exhibit an increased O2 saturation
- The patient will be able to verbalize understanding of the use of O2 supplementation.
Nursing Assessment with Rationales:
- Assess the patient’s respiratory status. This will help the health care team identify any physiological changes.
- Assess the patient’s need of supplemental O2. This will help monitor if changes need to be made to the plan of care.
- Assess the patient’s current activity levels. The will help to identify the patient’s limitations and abilities.
Nursing Interventions and Rationales:
- Check the patient’s breathing rate, characteristics, including the involvement of accessory muscles when breathing, and any other irregular breathing patterns. Auscultate the lungs and monitor for adventitious breath sounds. To establish a baseline. Gas exchange is affected by rapid and shallow breathing patterns, as well as hypoventilation. Hypoxia, on the other hand, is characterized by an increased respiratory rate, the employment of accessory muscles, nasal flaring, diaphragm breathing, and a panicky appearance in the patient’s eyes.
- Watch out for nail beds and skin cyanosis, as well as the color of the tongue and oral mucous membranes. Central cyanosis of the tongue and oral mucosa signals severe hypoxia and requires immediate medical attention, whereas peripheral cyanosis of the extremities may or may not be significant.
- Constantly monitor the patient’s oxygen saturation through a pulse oximeter. Pulse oximetry is an effective method for detecting oxygenation abnormalities. Significant oxygenation concerns are indicated by an oxygen saturation of less than 90% or a partial pressure of oxygen of less than 80.
- Constantly check the results of blood chemistry and arterial blood gases (ABG). Elevated Carbon dioxide levels and diminishing levels of oxygen may indicate respiratory acidosis and hypoxemia (low level of blood oxygen, particularly in the arteries).
- Place the patient in a high or semi-Fowler’s position with the head of the bed elevated. Also, encourage the patient to sit in an upright position if tolerated. Improved thoracic capacity, complete diaphragm fall, and increased lung expansion prevent abdominal contents from crowding when placing the patient in the upright or semi-Fowler’s position.
- Analyze the influence of shifting positions on ABGs and pulse oximetry readings. Ventilation and perfusion imbalances are aggravated by positioning the patient’s most impaired lung regions in the dependent position, where perfusion is greatest.
Risk for Infection
Risk for Infection occures because the increased fluid in the pleural cavity can cause bacterial growth leading to infection.
Nursing Diagnosis: Risk for infection
Related To:
- Increased fluid in pleural space
- Disease Process
As Evidenced By:
- As a risk nursing diagnosis, the Risk for Infection is entirely unrelated to any signs and symptoms since it has not yet developed in the patient, and safety precautions will be initiated instead.
Expected Outcomes:
- The patient will show no signs of infection
- The patient is able to state infection prevention strategies
Nursing Assessment with Rationales:
- Assess vital signs. This will help identify physiological changes that occur with infection
- Assess the patient’s infection prevention knowledge. It is important to assess the patient’s level of understanding of infection prevention.
- Assess the patient’s labs, especially the CBC (WBC count). This will help identify what interventions will be needed in the patient’s plan of care.
Nursing Interventions and Rationales:
- Keep an eye on the white blood cell count (WBC) of the patient. The normal WBC count is between 4,500 and 11,000 cells per microliter. Although the infection may be present without an elevated WBC count in older people, a rising white blood cell count reflects the body’s attempts to fight infections. On the other hand, a very low WBC count could also suggest a high risk of infection.
- Closely monitor the color and characteristics of the patient’s respiratory secretions. Sputum that is thick, yellow, green, or tan-colored could suggest infection. It is possible that a sputum culture will be required by the attending physician.
- Consider the patient’s dietary requirements. Weight and laboratory parameters, such as serum albumin, should be monitored. Malnutrition has an impact on the development of immune cells, which are essential for fighting off infections.
- Wash hands frequently or performs hand hygiene before making contact with the patient. Instruct also the patient and their family members on these responsibilities and let them be aware of when hand hygiene is required. Microorganisms are effectively removed from hands using friction and running water. It is better to use antimicrobial soap than plain soap at reducing bacterial counts, while alcohol-based hand rubs are the most ideal. Between procedures, washing minimizes the chance of infections spreading from one part of the body to another. Handwashing frequently is intended to break the infection cycle. When handling a delicate site of entry, such as changing a central line dressing, catheter care, or incision care, maintaining clean hands and aseptic practices reduces the chance of transferring bacteria into the body. Hand hygiene is the most essential factor for avoiding infections.
- Advise the patient to eat a well-balanced meal that is high in protein and calories. Good nutrition and a well-balanced diet strengthen the immune system’s response and the functioning of all body systems.
- Highly encourage coughing and deep breathing techniques every two hours, as well as frequent position changes. These techniques contribute to the lowering of secretion stasis in the lungs. When there are stagnant lung secretions, the respiratory tract becomes infected with bacteria, which can lead to another lung disease.
More Pleural Effusion Nursing Diagnosis
Nursing References
Ackley, B. J., Ladwig, G. B., Makic, M. B., Martinez-Kratz, M. R., & Zanotti, M. (2020). Nursing diagnoses handbook: An evidence-based guide to planning care. St. Louis, MO: Elsevier.
Alizadeh, A., Dyck, S. M., & Karimi-Abdolrezaee, S. (2019). Traumatic Spinal Cord Injury: An Overview of Pathophysiology, Models and Acute Injury Mechanisms. Frontiers in neurology, 10, 282. https://doi.org/10.3389/fneur.2019.00282
Gulanick, M., & Myers, J. L. (2017). Nursing care plans: Diagnoses, interventions, & outcomes. St. Louis, MO: Elsevier.
Hills, Teresa E. MSN, RN, ACNP-BC, CNRN. Caring for patients with a traumatic spinal cord injury. Nursing 50(12):p 30-40, December 2020. | DOI: 10.1097/01.NURSE.0000721724.96678.5a
Ignatavicius, D. D., Workman, M. L., Rebar, C. R., & Heimgartner, N. M. (2018). Medical-surgical nursing: Concepts for interprofessional collaborative care. St. Louis, MO: Elsevier.
Silvestri, L. A. (2020). Saunders comprehensive review for the NCLEX-RN examination. St. Louis, MO: Elsevier.
Best Nursing Books and Resources
These are the nursing books and resources that we recommend.
NurseStudy.net is a participant in the Amazon Services LLC Associates Program. Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. Please see our Privacy Policy

The Nursing Diagnosis Handbook E-Book: An Evidence-Based Guide to Planning Care
This is an excellent reference for nurses and nursing students. While it is a great resource for writing nursing care plans and nursing diagnoses, it also helps guide the nurse to match the nursing diagnosis to the patient assessment and diagnosis.
This handbook has been updated with NANDA-I approved Nursing Diagnoses that incorporates NOC and NIC taxonomies and evidenced based nursing interventions and much more.
NANDA International Nursing Diagnoses: Definitions & Classification, 2021-2023
All introductory chapters in this updated version of a ground-breaking text have been completely rewritten to give nurses the knowledge they require to appreciate assessment, its relationship to diagnosis and clinical reasoning, and the goal and use of taxonomic organization at the bedside.
Nursing Care Plans: Nursing Diagnosis and Intervention
It contains more than 200 care plans that adhere to the newest evidence-based recommendations.
Additionally, it distinguishes between nursing and collaborative approaches and highlights QSEN competencies.
Best Nursing Books and Resources
These are the nursing books and resources that we recommend.
NurseStudy.net is a participant in the Amazon Services LLC Associates Program. Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. Please see our Privacy Policy

The Nursing Diagnosis Handbook E-Book: An Evidence-Based Guide to Planning Care
This is an excellent reference for nurses and nursing students. While it is a great resource for writing nursing care plans and nursing diagnoses, it also helps guide the nurse to match the nursing diagnosis to the patient assessment and diagnosis.
This handbook has been updated with NANDA-I approved Nursing Diagnoses that incorporates NOC and NIC taxonomies and evidenced based nursing interventions and much more.
NANDA International Nursing Diagnoses: Definitions & Classification, 2021-2023
All introductory chapters in this updated version of a ground-breaking text have been completely rewritten to give nurses the knowledge they require to appreciate assessment, its relationship to diagnosis and clinical reasoning, and the goal and use of taxonomic organization at the bedside.
Nursing Care Plans: Nursing Diagnosis and Intervention
It contains more than 200 care plans that adhere to the newest evidence-based recommendations.
Additionally, it distinguishes between nursing and collaborative approaches and highlights QSEN competencies.
Disclaimer:
Please follow your facilities guidelines and policies and procedures.
The medical information on this site is provided as an information resource only and is not to be used or relied on for any diagnostic or treatment purposes.
This information is not intended to be nursing education and should not be used as a substitute for professional diagnosis and treatment.


