Last updated on January 27th, 2024 at 04:10 pm
Definition
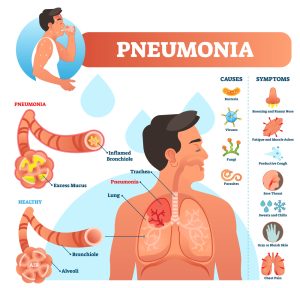
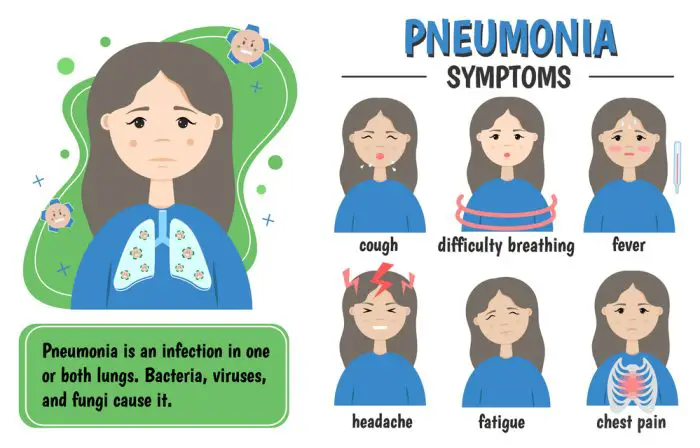
Pneumonia is an inflammatory condition affecting the lung parenchyma—specifically the alveoli and the bronchioles. It can be caused by various microorganisms, including bacteria, viruses, and fungi.
Signs and Symptoms
Subjective:
- Complaints of chest pain or discomfort
- Fatigue or weakness
- Shortness of breath (SOB), especially during physical activity
- Chills or fever
- Cough, with or without phlegm
- General malaise
Objective:
- Fever
- Increased respiratory rate
- Crackles or wheezing
- Decreased oxygen saturation O2 sat
- Productive cough
Related Factors and At-Risk Population
- Recent respiratory tract infection
- Chronic respiratory conditions, like COPD or asthma
- Smoking
- Immune system suppression
- Elderly individuals
- Children under the age of 2
- Individuals with chronic illnesses
- Immunosuppressed individuals
Nursing Diagnosis for Pneumonia
Below are five nursing diagnoses that can be used for Pneumonia Nursing Care Plans.
- Ineffective airway clearance related to increased mucus production.
- Impaired gas exchange related to alveolar consolidation.
- Activity intolerance related to decreased oxygenation.
- Acute pain related to inflammation and irritation of the pleura.
- Risk for infection related to compromised immune system or existing co-morbidities.
Desired Outcomes:
- Improved respiratory function.
- Clear breath sounds.
- Absence of chest pain or discomfort.
- Normal oxygen saturation levels.
- Absence of fever and other symptoms of infection.
Nursing Interventions for Pneumonia
- Position the patient upright or in a high Fowler’s position. Rationale: This promotes lung expansion and facilitates easier breathing.
- Administer prescribed antibiotics or antiviral medications. Rationale: Helps to treat the underlying cause of the pneumonia.
- Encourage deep breathing exercises and the use of incentive spirometry. Rationale: Promotes lung expansion and mucus clearance.
- Administer oxygen therapy as prescribed. Rationale: Increases oxygen saturation and supports respiratory function.
- Monitor vital signs, specifically respiratory rate and oxygen saturation. Rationale: Allows for timely detection of respiratory distress or deterioration.
- Encourage fluid intake. Rationale: It helps to thin out secretions, making it easier to cough them up.
Nursing Care Plan for Pneumonia
Ineffective Airway Clearance
Nursing Diagnosis: Ineffective airway clearance related to increased production of secretions secondary to pneumonia.
Related factors/causes:
- Accumulation of purulent secretions in the bronchi and bronchioles.
- Bronchospasm resulting from inflammation.
- Fatigue and muscle weakness affecting the efficiency of coughing.
Desired Outcomes:
- The patient will demonstrate effective coughing and expectorate secretions without signs of respiratory distress.
- Breath sounds will improve, becoming clearer on auscultation.
- Oxygen saturation will remain within normal limits for the patient’s age and condition.
Nursing Interventions with Rationales:
- Position the patient in an upright or high Fowler’s position.
- Rationale: This promotes lung expansion and gravity assists in draining secretions from the lower parts of the lungs, facilitating easier breathing and expectoration.
- Encourage deep breathing exercises and the use of incentive spirometry every 1-2 hours while awake.
- Rationale: Regular deep breathing promotes lung expansion and helps mobilize secretions. The incentive spirometer provides visual feedback to the patient, encouraging deeper breaths and aiding in preventing atelectasis (collapse of lung alveoli).
- Administer prescribed mucolytic agents or nebulizer treatments, and ensure adequate hydration.
- Rationale: Mucolytic agents help break down thick mucus, making it easier to expectorate. Nebulized treatments can help reduce inflammation and bronchospasm. Adequate hydration helps to thin out secretions, further facilitating their removal.
Impaired Gas Exchange
Nursing Diagnosis: Impaired gas exchange related to alveolar consolidation and decreased oxygen diffusion secondary to pneumonia.
Related factors/causes:
- Accumulation of secretions and pus in the alveoli.
- Alveolar wall inflammation causing thickening, which limits gaseous exchange.
- Hypoventilation related to pain, fatigue, or bronchospasm.
Desired Outcomes:
- The patient will maintain oxygen saturation within the normal range for their age and condition.
- The patient will express feelings of decreased breathlessness and improved respiratory comfort.
- Arterial blood gas (ABG) values will be within normal limits.
Nursing Interventions with Rationales:
- Administer supplemental oxygen as prescribed.
- Rationale: Supplemental oxygen enhances the concentration of oxygen available for diffusion into the blood, supporting the achievement of optimal oxygen saturation levels.
- Position the patient in a semi-Fowler’s to high Fowler’s position.
- Rationale: Elevating the head and chest promotes maximum lung expansion, reducing shunting of blood through poorly ventilated areas of the lung. This aids in improving ventilation-perfusion matching and enhances gaseous exchange.
- Regularly monitor ABGs, oxygen saturation, and other vital signs, adjusting interventions as needed.
- Rationale: Continuous monitoring allows for timely identification of deteriorating gas exchange, enabling quick interventions. Early detection and management can prevent complications and enhance the effectiveness of therapeutic measures.
Nursing Test Questions for Pneumonia
Question 1: A nurse is assessing a patient suspected of having pneumonia. Which of the following clinical manifestations would most likely support this diagnosis? A. Bradypnea and dry cough B. Elevated blood pressure and bradycardia C. Clear lung sounds bilaterally D. Crackles on lung auscultation and fever
Answer: D. Crackles on lung auscultation and fever
Rationale: Crackles on auscultation indicate the presence of secretions in the alveoli, which is consistent with pneumonia. Fever is a systemic response to infection. The other options are not specific signs of pneumonia.
Question 2: Which of the following patients is at the highest risk for developing pneumonia? A. A 30-year-old marathon runner with allergies B. A 65-year-old smoker with chronic obstructive pulmonary disease (COPD) C. A 40-year-old yoga instructor who recently had a flu vaccine D. A 22-year-old college student who drinks alcohol occasionally
Answer: B. A 65-year-old smoker with chronic obstructive pulmonary disease (COPD)
Rationale: Smoking and COPD are significant risk factors for pneumonia because they compromise the lung’s defense mechanisms. The other individuals do not have factors that increase their risk to the same extent.
Question 3: A patient with pneumonia is prescribed antibiotic therapy. Which nursing intervention is the highest priority? A. Encouraging fluid intake B. Administering the antibiotic on schedule C. Teaching the patient about the side effects of the antibiotic D. Promoting bed rest
Answer: B. Administering the antibiotic on schedule
Rationale: While all the options are essential interventions for a patient with pneumonia, timely administration of the prescribed antibiotic is crucial to effectively treat the infection and prevent complications.
Question 4: A nursing student is asked to explain the pathophysiology of pneumonia. Which of the following explanations indicates a correct understanding? A. “Pneumonia is caused by the inhalation of large particles that irritate the bronchioles.” B. “Pneumonia develops when the alveoli fill with blood, preventing air exchange.” C. “It results from the inhalation of harmful microorganisms that multiply and cause inflammation in the alveoli.” D. “Pneumonia is primarily a cardiac condition affecting the heart’s ability to pump oxygen.”
Answer: C. “It results from the inhalation of harmful microorganisms that multiply and cause inflammation in the alveoli.”
Rationale: Pneumonia is primarily a respiratory condition wherein microorganisms cause infection and inflammation within the alveoli. The alveoli become filled with pus and other liquid, making oxygen exchange difficult.
Question 5: A nurse is caring for a patient with pneumonia. The nurse identifies ineffective airway clearance. Which of the following would be an appropriate nursing intervention for this problem? A. Encouraging the patient to lie flat B. Restricting fluid intake to decrease secretions C. Encouraging deep breathing and coughing exercises D. Advising the patient to suppress cough to prevent fatigue
Answer: C. Encouraging deep breathing and coughing exercises
Rationale: Deep breathing and coughing exercises help in mobilizing and expectorating secretions, improving airway clearance. The other options would potentially worsen the patient’s condition or are not directly related to improving airway clearance.
Nursing References
Ackley, B. J., Ladwig, G. B., Makic, M. B., Martinez-Kratz, M. R., & Zanotti, M. (2020). Nursing diagnoses handbook: An evidence-based guide to planning care. St. Louis, MO: Elsevier.
Cason, C. L., Tyner, T., Saunders, S., & Broome, L. (2007). Nurses’ implementation of guidelines for ventilator-associated pneumonia from the Centers for Disease Control and Prevention. American journal of critical care, 16(1), 28-37.
Eshwara, Vandana Kalwaje1,; Mukhopadhyay, Chiranjay1; Rello, Jordi2,3. Community-acquired bacterial pneumonia in adults: An update. Indian Journal of Medical Research 151(4):p 287-302, April 2020. | DOI: 10.4103/ijmr.IJMR_1678_19
Grief, S. N., & Loza, J. K. (2018). Guidelines for the Evaluation and Treatment of Pneumonia. Primary care, 45(3), 485–503. https://doi.org/10.1016/j.pop.2018.04.001
Gulanick, M., & Myers, J. L. (2022). Nursing care plans: Diagnoses, interventions, & outcomes. St. Louis, MO: Elsevier.
Ignatavicius, D. D., Workman, M. L., Rebar, C. R., & Heimgartner, N. M. (2020). Medical-surgical nursing: Concepts for interprofessional collaborative care. St. Louis, MO: Elsevier.
Lim W. S. (2022). Pneumonia—Overview. Encyclopedia of Respiratory Medicine, 185–197. https://doi.org/10.1016/B978-0-12-801238-3.11636-8
Lim WS, Macfarlane JT, Boswell TCJ, et al Study of community acquired pneumonia aetiology (SCAPA) in adults admitted to hospital: implications for management guidelines Thorax 2001;56:296-301.
Silvestri, L. A. (2020). Saunders comprehensive review for the NCLEX-RN examination. St. Louis, MO: Elsevier.
Best Nursing Books and Resources
These are the nursing books and resources that we recommend.
NurseStudy.net is a participant in the Amazon Services LLC Associates Program. Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. Please see our Privacy Policy

The Nursing Diagnosis Handbook E-Book: An Evidence-Based Guide to Planning Care
This is an excellent reference for nurses and nursing students. While it is a great resource for writing nursing care plans and nursing diagnoses, it also helps guide the nurse to match the nursing diagnosis to the patient assessment and diagnosis.
This handbook has been updated with NANDA-I approved Nursing Diagnoses that incorporates NOC and NIC taxonomies and evidenced based nursing interventions and much more.
NANDA International Nursing Diagnoses: Definitions & Classification, 2021-2023
All introductory chapters in this updated version of a ground-breaking text have been completely rewritten to give nurses the knowledge they require to appreciate assessment, its relationship to diagnosis and clinical reasoning, and the goal and use of taxonomic organization at the bedside.
Nursing Care Plans: Nursing Diagnosis and Intervention
It contains more than 200 care plans that adhere to the newest evidence-based recommendations.
Additionally, it distinguishes between nursing and collaborative approaches and highlights QSEN competencies.
Disclaimer
Please follow your facility’s guidelines, policies, and procedures.
The medical information on this site is provided as an information resource only and is not to be used or relied on for diagnostic or treatment purposes.
This information is intended to be nursing education and should not be used as a substitute for professional diagnosis and treatment.


Superb hope to learn more