Hypertension, or high blood pressure, is a silent but dangerous condition affecting millions of people worldwide. As a nurse, understanding the complexity of hypertension and its management is crucial to ensuring the well-being of your patients.
This comprehensive guide will walk you through the nursing care plan approach, a method that empowers healthcare professionals to provide the highest level of care, including the nursing diagnosis for hypertension.
In this guide, we’ll delve into the causes, risk factors, symptoms, and complications of hypertension, explore the importance of nursing assessment and diagnosis, discuss how to develop care plans with a focus on nursing diagnosis for hypertension, and share valuable resources and tools to help you create effective care plans for your patients. Together, we can make a difference in the lives of those affected by hypertension.
Short Summary
- Understanding the causes, symptoms and complications of hypertension is essential for healthcare professionals to provide optimal care.
- Nurses play an important role in assessing risk factors, developing personalized care plans, and providing interventions to improve patient health outcomes.
- Patient education and support are key components of successful management of hypertension through lifestyle modifications such as diet changes, exercise regimens or quitting smoking.
Understanding Hypertension
Hypertension, commonly known as high blood pressure, is a medical condition in which the force of the blood against the walls of the arteries is consistently too high.
This increased pressure can lead to serious health complications, such as organ damage, stroke, and heart attack. Understanding the causes, risk factors, symptoms, and potential complications of hypertension is essential for nurses to provide the best possible care for their patients.
Hypertension is a multifactorial condition, with various causes and risk factors contributing to its development, such as age, ethnicity, family history, lifestyle, increaed salt intake, and certain medical conditions.
The symptoms of hypertension can be subtle or even nonexistent, earning it the nickname “the silent killer.” However, when symptoms do present, they may include headaches, breathlessness, nosebleeds, chest pain, blurred vision, dizziness, and weariness.
It is crucial for healthcare professionals to recognize these signs to provide timely and appropriate interventions.
Causes and Risk Factors
Increased sympathetic nervous system activity, renal sodium reabsorption, activity of the renin-angiotensin-aldosterone system, impaired vasodilation, insulin resistance, and immune response activation all influence the development of hypertension.
Identifying modifiable risk factors can help reduce the risk of hypertension. Furthermore, a sedentary lifestyle can lead to an elevated heart rate, causing the heart to work harder and potentially contribute to hypertension.
Secondary hypertension, a type of high blood pressure caused by an underlying condition, can arise from various factors such as kidney, adrenal, or thyroid issues, congenital blood vessel defects, sleep apnea, certain medications, street drugs, tobacco, and excessive alcohol use.
Identifying and addressing these causes can significantly improve blood pressure control and overall health outcomes.
Symptoms and Complications
As mentioned earlier, hypertension is often referred to as the “silent killer” since it typically does not manifest any symptoms. However, in some cases, individuals with hypertension may experience headaches, breathlessness, nosebleeds, chest pain, blurred vision, dizziness, and difficulty sleeping.
It is essential to recognize these signs and symptoms promptly to initiate appropriate interventions and prevent further complications.
Untreated hypertension can have severe complications. These include vascular damage, heart failure, kidney dysfunction, nocturia, angina, myocardial infarction, left ventricular hypertrophy and cerebrovascular complications such as transient ischemic attacks or strokes.
Timely diagnosis and treatment are crucial to mitigate these risks and maintain the patient’s health and quality of life.
Treatment for Hypertension
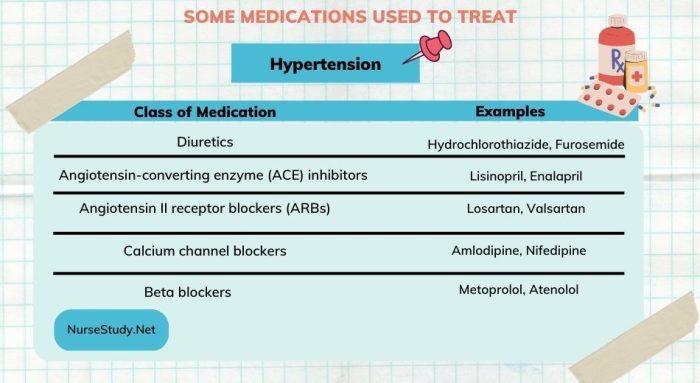
Medications. The primary treatment for hypertension is the use of anti-hypertensive medications. The category or type of drugs depend on your average blood pressure reading, underlying conditions, and complications.
- Thiazide diuretics (e.g. hydrochlorothiazide) – eliminate sodium and water through urine, leading to a decline in blood volume
- Angiotensin-converting enzyme (ACE) inhibitors (e.g. lisinopril) – block the formation of angiotensin, a peptide hormone that narrows blood vessels, leading to vasodilation
- Angiotensin II receptor blockers (ARBs) (e.g. losartan) – block the action of angiotensin, leading to vasodilation
- Calcium channel blockers (e.g. amolodipine and diltiazem) – promote vasodilation and reduction of heart rate. Grapefruit juice is contraindicated for patients on Calcium channel blockers.
- Alpha blockers (e.g. doxazosin) – reduce the effect of angiotensin by decreasing the nerve impulses to the blood vessels
- Alpha-beta blockers (e.g. carvedilol) – slow down the heartbeat, leading to reduction of cardiac workload
- Beta blockers (e.g. atenolol) – open the blood vessels and reduces cardiac workload
- Aldosterone antagonists (e.g. spironolactone) – block aldosterone, a hormone that promotes retention of salt and fluid which lead to high blood pressure
- Renin inhibitors (e.g. aliskiren) – reduce the production of an enzyme called renin in the kidneys, leading to decreased blood pressure. These should not be combined with ARBs or ACE inhibitors due to increased risk for stroke
- Vasodilators (e.g. hydralazine) – directly dilates the arterial walls
- Central-acting agents (e.g. clonidine) – helps block brain-to-nervous system signaling in terms of narrowing blood vessels and increasing heart rate
Nursing Assessment and Diagnosis
Nursing assessment and diagnosis play a vital role in identifying risk factors and crafting personalized interventions for hypertension patients.
By understanding the unique needs and challenges of each patient, nurses can develop comprehensive care plans that effectively address the underlying causes and contributing factors of hypertension.
Common nursing diagnoses associated with hypertension include decreased cardiac output, ineffective coping, and activity intolerance.
By accurately assessing a patient’s condition and risk factors, nurses can develop targeted interventions and strategies to help patients manage their hypertension and improve their overall health outcomes.
Identifying Risk Factors
Risk factors for hypertension include unhealthy diets, lack of physical activity, high sodium intake, low potassium intake, obesity, regular alcohol consumption, stress, age, family history, genetics, race, and sex. Nurses play a crucial role in identifying these risk factors and helping patients understand their significance in the development and progression of hypertension.
Apart from the regular risk factors, certain others including heightened sympathetic nervous system activity, renal sodium reabsorption, renin-angiotensin-aldosterone system functioning, lower vasodilation rate, insulin resistance, and immune response activation also have a role to play in hypertension development. Understanding these underlying mechanisms can help nurses provide more effective care and support for patients with hypertension.
Nursing Diagnoses for Hypertension
Nursing diagnoses for hypertension patients are crucial for providing targeted care and support. Some common nursing diagnoses include decreased cardiac output, ineffective coping, and activity intolerance. Formulating a nursing diagnosis involves considering all potential causes of hypertension, such as stress and high cholesterol, and identifying the specific factors contributing to the patient’s condition.
For example, a nursing diagnosis for a patient with hypertension might be “ineffective coping leading to high stress levels, resulting in high blood pressure.” By accurately identifying the contributing factors and addressing them through targeted interventions, nurses can help patients manage their hypertension more effectively and improve their overall health outcomes.
Developing Hypertension Care Plans
Developing care plans for hypertension patients is a vital part of the nursing process. Care plans involve setting goals and expected outcomes for each patient, as well as implementing interventions to help them achieve these goals. Interventions may include patient education, lifestyle modifications, and medication adherence.
By creating individualized care plans tailored to each patient’s unique needs, nurses can provide comprehensive support and guidance for hypertension management. This not only helps patients achieve better blood pressure control, but also reduces the risk of complications and improves their overall quality of life.
Setting Goals and Expected Outcomes
When developing a care plan for a hypertension patient, it is essential to set realistic and achievable goals and expected outcomes. These may include effectively, safely, and economically lowering and controlling blood pressure, promoting optimal blood pressure levels, and reducing the risk of health problems caused by high blood pressure. Nurses should also consider the patient’s individual needs, preferences, and potential barriers to change when setting goals.
It is important to note that for patients with chronically elevated blood pressure or hypertensive crisis, blood pressure should be lowered gradually to prevent symptoms of hypotension at even regular blood pressure levels. Ensuring that patients adhere to their treatment regimen and receive appropriate support is crucial to achieving these goals.
Implementing Interventions
Interventions for hypertension patients may vary depending on their individual needs and goals. However, some common interventions include patient education, lifestyle modifications, and medication adherence. Nurses can assist patients in recognizing their individual risk factors, instruct them in how to measure their blood pressure, offer encouragement, and examine medications attentively.
In some cases, patients may require additional interventions, such as assistance to lose weight and the use of diuretics to eliminate excess fluid from the body if they are exhibiting symptoms like shortness of breath or extremely elevated blood pressure.
Ultimately, the goal of implementing interventions is to help patients achieve better blood pressure control and reduce the risk of complications associated with hypertension.
Addressing Common Nursing Diagnoses in Hypertension
Nurses play a critical role in addressing common nursing diagnoses in hypertension patients, such as decreased cardiac output, ineffective coping, and activity intolerance. By assessing the patient’s condition and providing appropriate interventions, nurses can help patients manage their hypertension more effectively and improve their overall health outcomes.
In this section, we will discuss each of these common nursing diagnoses in more detail and provide guidance on how nurses can address them in their practice.
Decreased Cardiac Output
Decreased cardiac output is a nursing diagnosis that refers to a condition where the heart is unable to provide an adequate amount of blood to meet the body’s requirements. In the context of hypertension, decreased cardiac output can result from vasoconstriction caused by chronic hypertension and vessel resistance.
Nurses can address this diagnosis by implementing interventions aimed at reducing the patient’s cardiac workload and improving blood flow. For example, raising edematous extremities above the level of the heart can assist in circulation and prevent skin damage.
Additionally, nurses should educate patients on the importance of adhering to their prescribed medication regimen, as uncontrolled blood pressure is the most prevalent cause of a hypertensive crisis and hypertensive emergencies.
Ineffective Coping
Ineffective coping is a nursing diagnosis that refers to an individual’s inability to manage stressors in a healthy manner, which may lead to difficulty managing daily stress and anxiety, changes in concentration, sleep pattern, communication pattern, fatigue, and lack of social support.
To address this diagnosis, nurses can provide patients with resources and support to help them develop healthy coping strategies. This may include teaching relaxation techniques, recommending support groups or counseling services, and encouraging patients to engage in activities that promote mental well-being.
By improving their coping skills, patients can better manage their stress levels and, in turn, their hypertension.
Activity Intolerance
Activity intolerance is a nursing diagnosis that refers to an insufficient amount of physiological or psychological energy to be able to complete or endure the daily activities that are required or desired. In the context of hypertension, patients may experience fatigue due to factors such as age, frailty, acute or chronic illness, heart failure, and hypothyroidism.
Nurses can assess a patient’s response to activity by evaluating their pulse rate, blood pressure, dyspnea or chest pain, excessive fatigue and weakness, diaphoresis, and dizziness or syncope.
To address activity intolerance, nurses can teach patients energy-conserving techniques and motivate progressive activity and self-care when tolerated. This will help to enhance hypertension patients’ capacity to participate in activities and improve their overall health outcomes.
Patient Education and Support
Patient education and support are essential components of successful hypertension management. As healthcare professionals, nurses play a critical role in educating patients about their condition, providing guidance on lifestyle modifications, and ensuring that patients adhere to their prescribed treatment regimens.
In this section, we will discuss the importance of patient education and support in more detail and provide guidance on how nurses can effectively educate patients on hypertension and promote lifestyle changes that may help improve their blood pressure control.
Educating Patients on Hypertension
Educating patients on hypertension is crucial, as it enables them to understand their condition, make informed decisions, and actively participate in their treatment. Nurses should provide patients with information about hypertension and its impact on the heart, blood vessels, kidneys, and brain, as well as discuss the importance of monitoring blood pressure and maintaining a “well-controlled” status.
Providing patient education materials, such as guides to lifestyle modification, and implementing educational programs in the fields of nutrition and physical activity, can be productive approaches to educating patients on hypertension. By empowering patients with the knowledge and tools they need to manage their condition, nurses can help improve health outcomes and quality of life for those living with hypertension.
Encouraging Lifestyle Changes
Lifestyle changes play a significant role in hypertension management, and nurses can encourage patients to adopt healthier habits to help manage their blood pressure. Some suggested lifestyle modifications include consuming a nutritious diet, engaging in regular physical activity, ceasing smoking, and adhering to prescribed medications.
Educating patients on their recommended daily sodium intake and suggesting low-sodium alternatives can also help regulate sodium and fluid intake. By providing support, encouragement, and resources, nurses can help patients make lasting lifestyle changes that will not only improve their hypertension management but also enhance their overall health and well-being.
Recommended Resources and Tools
In addition to the information provided in this guide, there are several recommended resources and tools available to help nurses create effective care plans for hypertension patients. These resources can assist nurses in developing comprehensive, personalized care plans that address the unique needs and challenges of each patient, ultimately improving health outcomes and quality of life.
In this section, we will discuss two key types of resources and tools: care plan templates and educational materials. These resources can help nurses create effective care plans and provide valuable information for both healthcare professionals and patients alike.
Care Plan Templates
Care plan templates for hypertension are documents that provide a structure for nurses to formulate personalized care plans for patients with hypertension. These templates can help streamline the care planning process, ensuring that all relevant information is considered and that each patient receives appropriate interventions based on their individual needs and goals.
Nurses can find care plan templates for hypertension on our nursing website. Utilizing these templates can save time and ensure a consistent approach to care planning for hypertension patients.
Educational Materials
Educational materials for hypertension include resources for health professionals, patient education materials, fact sheets, and guides for lifestyle changes such as diet and exercise.
These materials can help nurses stay up-to-date on the latest evidence-based guidelines, clinical practice guidelines, and research articles, as well as provide valuable information to patients on hypertension management.
Examples of patient education materials include brochures, pamphlets, and videos that provide an explanation of hypertension and its management, as well as fact sheets and guides for lifestyle modifications that focus on nutrition, physical activity, and stress management.
By providing these materials to patients, nurses can effectively educate and support them in their journey to better health and hypertension management.
3 Nursing Care Plans for Hypertension
One of the main goals for a nursing care plan for hypertension is to maintain blood pressure. The patieint and healthcare team should work together to lower blood pressure or control blood pressure.
Deficient Knowledge
Nursing Diagnosis: Deficient Knowledge related to new diagnosis of secondary hypertension as evidenced by patient’s verbalization of “I want to know more about my new diagnosis and care”
Desired Outcome: At the end of the health teaching session, the patient will be able to demonstrate sufficient knowledge of hypertension and its management.
Nursing Interventions for Deficient Knowledge
Assess the patient’s readiness to learn, misconceptions, and blocks to learning (e.g. denial of diagnosis or poor lifestyle habits). To address the patient’s cognition and mental status towards the new diagnosis of hypertension and to help the patient overcome blocks to learning.
Explain what hypertension is, its types (specifically secondary hypertension), and how it affects the vital organs such as the heart, kidneys, brain, and blood vessels. Avoid using medical jargons and explain in layman’s terms. To provide information on hypertension and its pathophysiology in the simplest way possible.
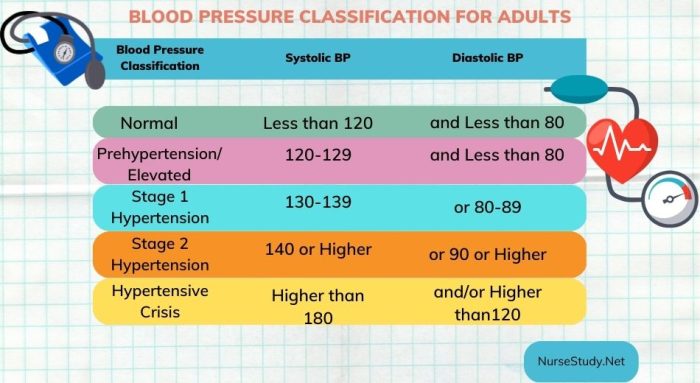
Teach the patient the stages of hypertension and set the target range for his/her blood pressure levels to be classified as “well-controlled”. To give the patient enough information on how to monitor blood pressure and the stages of hypertension and the desired limits of blood pressure levels.
Demonstrate how to perform blood pressure monitoring. To empower patient to monitor his/her blood pressure levels at home.
Inform the patient the details about the prescribed antihypertensive medications (e.g. drug class, use, benefits, side effects, and risks) to control hypertension, and explain how to properly self-administer each of them. Ask the patient to repeat or demonstrate the self-administration details to you. To inform the patient of each prescribed drug and to ensure that the patient fully understands the purpose, possible side effects, adverse events, and self-administration details.
Use open-ended questions to explore the patient’s lifestyle choices and behaviors that can be linked to the development of hypertension. Teach the patient on how to modify these risk factors (e.g. smoking, excessive alcohol intake, high sodium and/or cholesterol diet, obesity, sedentary lifestyle, etc). To assist the patient in identifying and managing modifiable risk factors related to hypertension.
Activity Intolerance
Nursing Diagnosis: Activity Intolerance related to sedentary lifestyle as evidenced by fatigue, generalized weakness, blood pressure level of 180/90, and shortness of breath upon exertion
Desired Outcome: The patient will participate in necessary and desired activities and demonstrate increase in activity levels.
Nursing Interventions for Activity Intolerance
Assess the patient’s activities of daily living, as well as actual and perceived limitations to physical activity. Ask for any form of exercise that he/she used to do or wants to try. To create a baseline of activity levels and mental status related to activity intolerance.
Encourage progressive activity through self-care and exercise as tolerated. Explain the need to reduce sedentary activities such as watching television and using social media over long periods. To gradually increase the patient’s tolerance to physical activity.
Refer the patient to physiotherapy / occupational therapy team as required. To provide a more specialized care for the patient in terms of helping him/her build confidence in increasing daily physical activity.
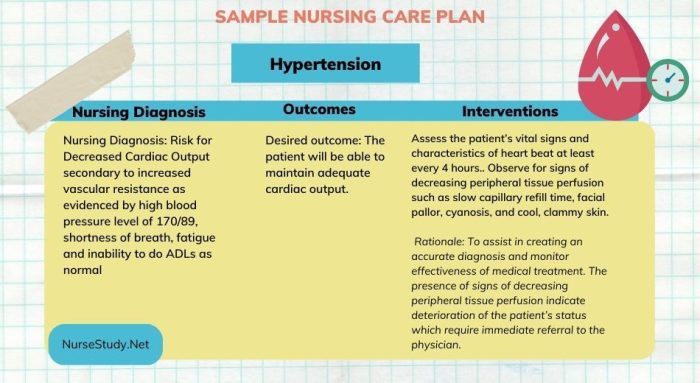
Decreased Cardiac Output
Nursing Diagnosis: Decreased cardiac output secondary to increased vascular resistance as evidenced by high blood pressure level of 180/90, shortness of breath, fatigue, and pounding in the chest and neck
Desired outcome: The patient will be able to maintain adequate cardiac output.
Nursing Interventions for Decreased Cardiac Output
Assess the patient’s vital signs and characteristics of heart beat at least every 4 hours. Observe for signs of decreasing peripheral tissue perfusion such as slow capillary refill, facial pallor, cyanosis, and cool, clammy skin. To assist in creating an accurate diagnosis and monitor effectiveness of medical treatment. The presence of signs of decreasing peripheral tissue perfusion indicate deterioration of the patient’s status which require immediate referral to the physician.
Administer prescribed medications for hypertension. The category or type of drugs depend on your average blood pressure reading, underlying conditions, and complications. These include vasodilators (direct or indirect), diuretics, and cardiac workload reducers.
Administer supplemental oxygen, as prescribed. Discontinue if SpO2 level is above the target range, or as ordered by the physician. To increase the oxygen level and achieve an SpO2 value within the target range.
Educate patient on stress management, deep breathing exercises, and relaxation techniques. Stress causes a persistent increase in cortisol levels, which has been linked to people with hypertension. Chronic stress may also cause an increase in adrenaline levels, which tend to increase the heart rate, respiratory rate, and blood sugar levels. Reducing stress is also an important aspect of dealing with fatigue.
Summary
In conclusion, managing hypertension effectively is vital to ensuring the well-being of patients and reducing the risk of serious health complications. This comprehensive guide has provided an overview of the nursing care plan approach to hypertension management, covering topics such as understanding hypertension, nursing assessment and diagnosis, developing care plans, addressing common nursing diagnoses, patient education and support, and recommended resources and tools.
As healthcare professionals, nurses play a crucial role in the management of hypertension. By understanding the complexities of this condition, providing personalized care plans, and offering ongoing support and education, nurses can make a significant difference in the lives of those affected by hypertension. Armed with the knowledge and resources provided in this guide, you are now better equipped to help your patients take control of their hypertension and improve their overall health and well-being.
Frequently Asked Questions
What is a good nursing diagnosis for hypertension?
A good nursing diagnosis would be risk for altered cardiovascular function related to excessive pressures within the blood vessels, presenting in the form of high blood pressure.
What are 3 examples of nursing diagnosis?
Three examples of nursing diagnosis are Risk for Impaired Skin Integrity, Urinary Retention and Decreased Cardiac Output. A medical diagnosis, on the other hand, is made by a physician or advanced health care practitioner.
Nurses use these diagnoses to develop individualized patient care plans.
What is the most common nursing diagnosis?
The most common nursing diagnosis is problem-focused, which is based on the signs and symptoms present in the patient. It is the easiest to identify due to its reliance on readily available information.
What blood pressure is a nursing diagnosis for hypotension?
A nursing diagnosis for hypotension is a blood pressure reading of less than 90/60 mmHg. Normal blood pressure for most adults is considered to be 120/80 mmHg, so readings below this level indicate hypotension.
See Also:
- Increased cerebral vascular pressure
- Pregnancy induced hypertension
- Heart failure
- Kidney disease
- Obstructive sleep apnea
Disclaimer
Please follow your facility’s guidelines, policies, and procedures.
The medical information on this site is provided as an information resource only and is not to be used or relied on for diagnostic or treatment purposes.
This information is intended to be nursing education and should not be used as a substitute for professional diagnosis and treatment.

