Ineffective coping is a nursing diagnosis that describes a situation where an individual cannot manage stressors effectively, leading to compromised well-being and health.
This diagnosis is crucial for nurses to identify and address, as it can significantly impact a patient’s overall health outcomes and quality of life.
Causes (Related to)
Ineffective coping can result from various factors that overwhelm an individual’s ability to manage stress. Common causes include:
- Situational crises
- Chronic illness or pain
- Mental health disorders
- Substance abuse
- Lack of social support
- Poor problem-solving skills
- Low self-esteem
- Cognitive impairment
- History of trauma or abuse
- Cultural or spiritual conflicts
Signs and Symptoms (As evidenced by)
Ineffective coping manifests through various signs and symptoms. During a physical assessment, a patient with ineffective coping may present with one or more of the following:
Subjective: (Patient reports)
- Feeling overwhelmed or unable to handle stress
- Difficulty making decisions
- Increased irritability or mood swings
- Sleep disturbances
- Loss of appetite or overeating
- Feelings of helplessness or hopelessness
- Difficulty concentrating
Objective: (Nurse assesses)
- Verbal expressions of inability to cope
- Destructive behavior towards self or others
- Social isolation or withdrawal
- Poor personal hygiene
- Neglect of responsibilities
- Impaired judgment
- Physical symptoms (e.g., headaches, muscle tension, fatigue)
- Use of ineffective coping mechanisms (e.g., substance abuse, avoidance)
Expected Outcomes
The following are common nursing care planning goals and expected outcomes for ineffective coping:
- The patient will verbalize understanding of effective coping strategies
- The patient will demonstrate the use of at least two new coping mechanisms
- The patient will report an improved ability to manage stress
- The patient will show reduced signs of anxiety or depression
- The patient will engage in self-care activities and maintain personal hygiene
- The patient will verbalize a more positive outlook on their situation
- The patient will participate in social activities and maintain relationships
- The patient will adhere to treatment plans and medication regimens (if applicable)
Nursing Assessment
The first step in nursing care is the assessment, during which the nurse gathers physical, psychosocial, emotional, and diagnostic data. The following section covers subjective and objective data related to ineffective coping.
- Conduct a comprehensive psychological assessment.
Evaluate the patient’s mental state, including mood, affect, thought processes, and cognitive function. This assessment helps identify underlying mental health issues contributing to ineffective coping. - Assess the patient’s current coping mechanisms.
Identify the patient’s current positive and negative coping strategies. This information guides the development of interventions to reinforce effective coping and address maladaptive behaviors. - Evaluate the patient’s support system.
Assess the availability and quality of the patient’s social support network, including family, friends, and community resources. Strong social support can significantly improve coping abilities. - Assess for signs of substance abuse.
Screen for the use of alcohol, drugs, or other substances as coping mechanisms. Substance abuse can exacerbate ineffective coping and lead to additional health problems. - Evaluate the patient’s stress level.
Use validated stress assessment tools to measure the patient’s perceived stress levels. This information helps gauge the severity of the coping issue and guides intervention planning. - Assess the patient’s physical health.
Conduct a physical examination to identify any underlying health issues that may be contributing to or resulting from ineffective coping. Chronic pain, fatigue, or other physical symptoms can impact coping abilities. - Evaluate the patient’s problem-solving skills.
Assess the patient’s ability to identify problems, generate solutions, and implement effective strategies. Poor problem-solving skills can contribute to ineffective coping. - Assess the patient’s spiritual and cultural beliefs
Understand the patient’s spiritual and cultural background, as these factors can influence coping strategies and overall well-being. - Review the patient’s medical history.
Examine the patient’s medical records for any previous diagnoses or treatments related to mental health or coping issues. This information provides context for the current situation and helps inform treatment planning.
Nursing Interventions
Nursing interventions are essential for helping patients develop effective coping strategies. The following section outlines possible nursing interventions for a patient with ineffective coping.
- Establish a therapeutic relationship.
Build rapport and trust with the patient to create a safe environment for discussing concerns and exploring coping strategies. Active listening and empathy are crucial in this process. - Provide education on stress management techniques.
Teach patients various stress reduction methods, such as deep breathing exercises, progressive muscle relaxation, mindfulness meditation, and guided imagery, and encourage regular practice of these techniques. - Promote healthy lifestyle habits.
Educate patients on the importance of regular exercise, balanced nutrition, adequate sleep, and avoiding harmful substances. These habits can significantly improve overall well-being and coping abilities. - Encourage the expression of feelings.
Provide opportunities for patients to express their emotions through talking, writing, or creative activities. This can help patients process their feelings and reduce emotional distress. - Teach problem-solving skills
Guide patients through problem-solving, including identifying problems, brainstorming solutions, evaluating options, and implementing chosen strategies. This empowers patients to address challenges more effectively. - Facilitate social support
Encourage patients to maintain and strengthen their social connections. Help identify potential sources of support and, if appropriate, provide information on support groups or community resources. - Implement cognitive-behavioral techniques
Teach patients to identify and challenge negative thought patterns and replace them with more balanced, realistic thoughts. This can help improve mood and coping abilities. - Provide crisis intervention as needed.
Be prepared to intervene in acute stress situations, offering immediate support and helping patients implement coping strategies to manage the crisis. - Collaborate with the healthcare team.
Work closely with other healthcare professionals, including mental health specialists, to ensure comprehensive care and coordinate referrals to appropriate services as needed. - Encourage self-care activities
Promote activities that enhance self-esteem and self-efficacy, such as engaging in hobbies, setting achievable goals, and practicing self-compassion. - Teach time management and organizational skills.
Help patients develop strategies for managing their time and responsibilities more effectively, reducing stress, and improving overall coping abilities. - Monitor medication compliance (if applicable)
If the patient is prescribed medications for mental health or related conditions, ensure proper adherence and educate about potential side effects and benefits.
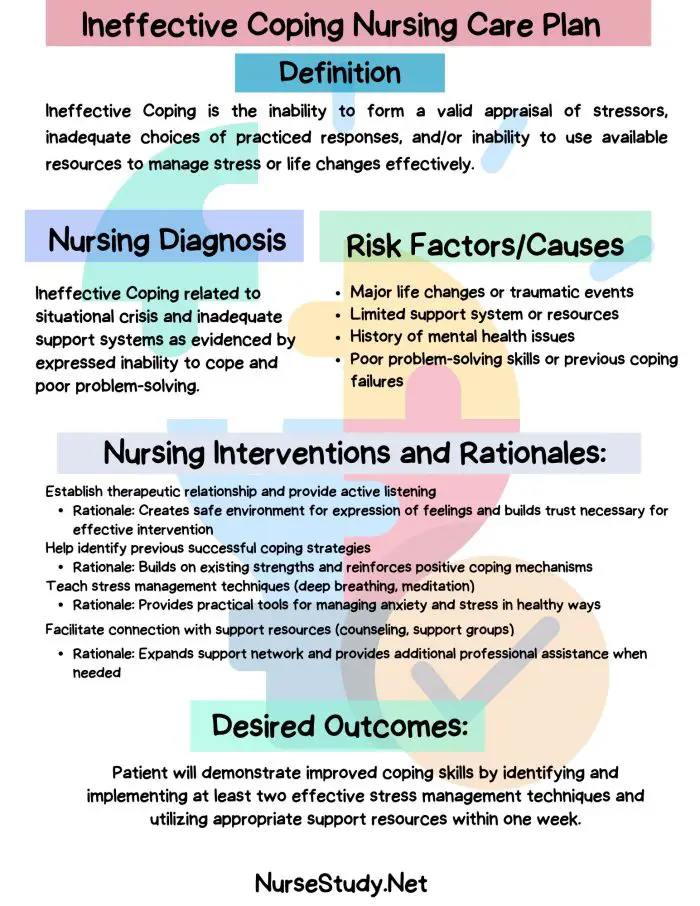
Nursing Care Plans
Ineffective Coping Nursing Diagnosis: Nursing care plans help prioritize assessments and interventions for both short and long-term goals of care. In the following section, you will find nursing care plan examples for ineffective coping.
Care Plan #1
Stress:
Ineffective coping related to overwhelming life stressors as evidenced by verbalized feelings of helplessness and increased anxiety.
Related factors/causes:
Recent job loss, financial strain, and lack of social support.
Nursing Interventions and Rationales:
- Assess the patient’s current coping mechanisms and stress levels.
Rationale: Provides baseline data for developing appropriate interventions. - Teach and practice stress reduction techniques (deep breathing, progressive muscle relaxation).
Rationale: Equips the patient with immediate tools to manage stress and anxiety. - Assist the patient in identifying and prioritizing current stressors.
Rationale: Helps break down overwhelming situations into manageable parts. - Encourage participation in support groups for individuals facing similar challenges.
Rationale: Provides a sense of community and shared experiences, reducing feelings of isolation. - Collaborate with a social worker to explore community resources for job search and financial assistance.
Rationale: Addresses practical concerns contributing to stress and ineffective coping.
Desired Outcomes:
- The patient will verbalize decreased feelings of helplessness within one week.
- The patient will demonstrate using at least two stress reduction techniques by discharge.
- The patient will identify at least one community resource for support by the end of the care period.
Care Plan #2
Chronic Pain:
Ineffective coping related to chronic pain as evidenced by verbal expressions of inability to manage pain and withdrawal from social activities.
Related factors/causes:
Persistent lower back pain, inadequate pain management strategies, and fear of movement.
Nursing Interventions and Rationales:
- Conduct a comprehensive pain assessment, including location, intensity, and aggravating/alleviating factors.
Rationale: Provides a clear understanding of the patient’s pain experience to guide interventions. - Educate the patient on non-pharmacological pain management techniques (e.g., heat/cold therapy, gentle exercises).
Rationale: Empowers the patient with additional tools for pain management beyond medication. - Collaborate with the healthcare team to optimize the pain management plan.
Rationale: Ensures a multidisciplinary approach to addressing chronic pain and its impact on coping. - Encourage a gradual increase in physical activity and social engagement.
Rationale: Helps overcome fear of movement and reduces social isolation, improving overall coping. - Teach cognitive-behavioral techniques for pain management (e.g., distraction, reframing negative thoughts).
Rationale: Addresses the psychological aspects of chronic pain and enhances coping strategies.
Desired Outcomes:
- The patient will report improved pain management using pharmacological and non-pharmacological methods within two weeks.
- The patient will demonstrate increased participation in daily activities by the end of the care period.
- The patient will verbalize at least two positive coping statements related to managing chronic pain by discharge.
Care Plan #3
Chronic Illness:
Ineffective coping related to a recent diagnosis of a chronic illness as evidenced by expressions of denial and refusal to discuss the condition.
Related factors/causes:
Recent diagnosis of Type 2 Diabetes, lack of knowledge about the condition, and fear of lifestyle changes.
Nursing Interventions and Rationales:
- Provide education about Type 2 Diabetes, including management strategies and potential complications.
Rationale: Increases patient’s understanding of the condition, reducing fear and promoting engagement in self-care. - Assess the patient’s readiness to learn and adapt to necessary lifestyle changes.
Rationale: Helps tailor interventions to the patient’s current emotional state and willingness to engage. - Introduce the patient to a diabetes support group or peer mentor program.
Rationale: Provides opportunities for shared experiences and learning from others facing similar challenges. - Teach problem-solving skills specific to diabetes management (e.g., meal planning, glucose monitoring).
Rationale: Empower the patient to participate in their care and develop effective coping strategies actively. - Collaborate with a dietitian to develop a personalized meal plan.
Rationale: Addresses specific dietary concerns and helps the patient feel more in control of their condition.
Desired Outcomes:
- The patient will verbalize acceptance of the diabetes diagnosis within two weeks.
- The patient will demonstrate proper use of glucose monitoring equipment by discharge.
- Patients will identify at least three lifestyle changes they are willing to implement by the end of the care period.
Care Plan #4
Post Traumatic Stress Disorder:
Ineffective coping related to symptoms of post-traumatic stress disorder (PTSD) as evidenced by hypervigilance, emotional outbursts, and social withdrawal.
Related factors/causes:
History of military combat exposure, untreated PTSD symptoms, and lack of mental health support.
Nursing Interventions and Rationales:
- Conduct a thorough assessment of PTSD symptoms and their impact on daily functioning.
Rationale: Provides a baseline for developing targeted interventions and monitoring progress. - Teach grounding techniques for managing flashbacks and anxiety (e.g., 5-4-3-2-1 sensory exercise).
Rationale: Equips the patient with immediate coping strategies for acute stress reactions. - Educate the patient about PTSD and its effects on thoughts, emotions, and behaviors.
Rationale: Increases understanding of symptoms, reducing self-blame and promoting self-compassion. - Facilitate referral to a mental health specialist for evidence-based PTSD treatments (e.g., cognitive processing therapy).
Rationale: Ensures access to specialized care for managing complex PTSD symptoms. - Encourage participation in a veterans’ support group or peer support program.
Rationale: Provides a safe space for sharing experiences and learning coping strategies from others with similar backgrounds.
Desired Outcomes:
- Patient will report a decrease in the frequency of flashbacks or intrusive thoughts within one month.
- Patient will demonstrate the use of at least two grounding techniques when experiencing anxiety by discharge.
- Patient will engage in at least one social activity per week by the end of the care period.
Care Plan #5
Substance Abuse:
Ineffective coping related to substance abuse as evidenced by continued use of alcohol despite adverse consequences and inability to manage stress without drinking.
Related factors/causes:
History of alcohol dependence, unresolved grief from the loss of a spouse, and lack of healthy coping mechanisms.
Nursing Interventions and Rationales:
- Assess the patient’s readiness for change using a validated tool (Stages of Change model).
Rationale: Helps tailor interventions to the patient’s current motivation level and willingness to address substance abuse. - Provide education on the effects of alcohol abuse on physical and mental health.
Rationale: Increases awareness of the consequences of continued substance use, potentially motivating change. - Teach and practice alternative stress management techniques (e.g., mindfulness meditation, exercise).
Rationale: Offers healthy alternatives to using alcohol as a coping mechanism. - Facilitate referral to addiction treatment services and support groups (e.g., Alcoholics Anonymous).
Rationale: Ensures access to specialized care and peer support for managing substance abuse. - Collaborate with a grief counselor to address unresolved loss and its connection to substance use.
Rationale: Addresses underlying emotional factors contributing to ineffective coping and substance abuse.
Desired Outcomes:
- The patient will verbalize willingness to explore alcohol-free coping strategies within one week.
- The patient will attend at least one support group meeting before discharge.
- By the end of the care period, the patient will demonstrate the use of at least two alternative stress management techniques.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
- Folkman, S., & Lazarus, R. S. (1988). Coping as a mediator of emotion. Journal of Personality and Social Psychology, 54(3), 466-475.
- Lazarus, R. S., & Folkman, S. (1984). Stress, appraisal, and coping. New York: Springer Publishing Company.
- National Institute of Mental Health. (2022). Post-Traumatic Stress Disorder. Retrieved from https://www.nimh.nih.gov/health/topics/post-traumatic-stress-disorder-ptsd
- Substance Abuse and Mental Health Services Administration. (2019). Enhancing Motivation for Change in Substance Use Disorder Treatment. Treatment Improvement Protocol (TIP) Series, No. 35. Rockville, MD: SAMHSA.
- World Health Organization. (2019). International statistical classification of diseases and related health problems (11th ed.). https://icd.who.int/
- Carpenito-Moyet, L. J. (2013). Nursing diagnosis: Application to clinical practice (14th ed.). Philadelphia: Lippincott Williams & Wilkins.
- Stuart, G. W. (2014). Principles and practice of psychiatric nursing (10th ed.). St. Louis, MO: Elsevier Mosby.
- Townsend, M. C., & Morgan, K. I. (2017). Psychiatric mental health nursing: Concepts of care in evidence-based practice (9th ed.). Philadelphia: F.A. Davis Company.