Gastrointestinal (GI) bleeding presents a critical nursing challenge requiring prompt assessment, intervention, and ongoing monitoring. This comprehensive guide explores the essential nursing diagnoses, interventions, and care plans necessary for effective patient care.
Understanding GI Bleeding
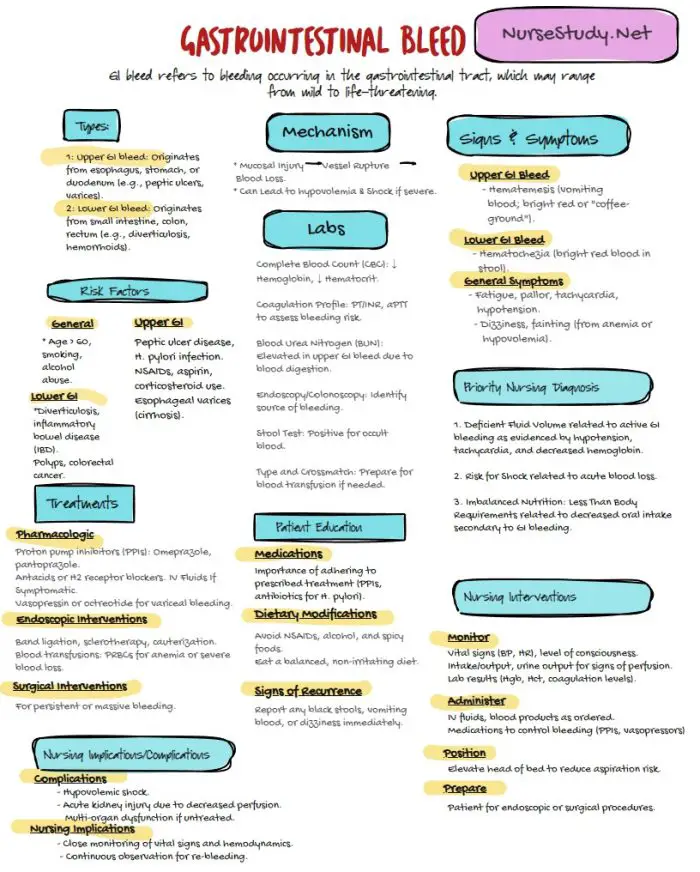
Gastrointestinal bleeding occurs anywhere along the digestive tract, from the esophagus to the rectum. The severity can range from mild to life-threatening, requiring immediate nursing intervention. The bleeding source may be either upper GI or lower GI tract.
Key Nursing Assessments
Physical Assessment
- Vital signs monitoring (blood pressure, heart rate, respiratory rate)
- Skin color and temperature
- Mental status
- Abdominal examination
- Stool characteristics
- Presence of hematemesis or melena
Diagnostic Monitoring
- Complete blood count (CBC)
- Coagulation profile
- Blood type and cross-match
- Stool occult blood test
- Monitoring for signs of shock
Primary Nursing Diagnoses and Care Plans
1. Risk for Shock
Nursing Diagnosis Statement:
Risk for Shock related to gastrointestinal bleeding evidenced by tachycardia, hypotension, and decreased tissue perfusion.
Related Factors/Causes:
- Active GI bleeding
- Volume depletion
- Decreased cardiac output
- Vasodilation
Nursing Interventions and Rationales:
Monitor vital signs every 15-30 minutes
- Rationale: Early detection of deterioration
Establish two large-bore IV access sites
- Rationale: Ensure rapid fluid resuscitation capability
Administer prescribed IV fluids and blood products
- Rationale: Restore blood volume and maintain tissue perfusion
Position patient in Trendelenburg if hypotensive
- Rationale: Improve cerebral perfusion
Monitor urine output hourly
- Rationale: Assess end-organ perfusion
Desired Outcomes:
- Stable vital signs
- Adequate tissue perfusion
- Normalized urine output
- Improved mental status
2. Impaired Gas Exchange
Nursing Diagnosis Statement:
Impaired Gas Exchange related to decreased hemoglobin concentration secondary to blood loss.
Related Factors/Causes:
- Decreased oxygen-carrying capacity
- Reduced hemoglobin levels
- Compromised tissue perfusion
Nursing Interventions and Rationales:
Monitor oxygen saturation continuously
- Rationale: Detect respiratory compromise early
Administer oxygen therapy as prescribed
- Rationale: Improve tissue oxygenation
Position patient for optimal breathing
- Rationale: Enhance pulmonary expansion
Monitor for signs of respiratory distress
- Rationale: Early intervention for deterioration
Desired Outcomes:
- Oxygen saturation >95%
- Normal respiratory rate
- Absence of dyspnea
- Improved energy levels
3. Deficient Fluid Volume
Nursing Diagnosis Statement:
Deficient Fluid Volume related to active GI bleeding evidenced by decreased blood pressure and tachycardia.
Related Factors/Causes:
- Ongoing blood loss
- Fluid shifts
- Decreased oral intake
- Altered coagulation
Nursing Interventions and Rationales:
Monitor fluid balance strictly
- Rationale: Track losses and replacement needs
Document intake and output hourly
- Rationale: Ensure adequate fluid replacement
Assess skin turgor and mucous membranes
- Rationale: Monitor hydration status
Administer blood products as ordered
- Rationale: Replace lost blood volume
Desired Outcomes:
- Balanced fluid status
- Stable vital signs
- Adequate urine output
- Moist mucous membranes
4. Acute Pain
Nursing Diagnosis Statement:
Acute Pain related to GI inflammation and bleeding evidenced by verbal reports and guarding behavior.
Related Factors/Causes:
- Mucosal inflammation
- Tissue ischemia
- Abdominal distention
- Gastric irritation
Nursing Interventions and Rationales:
Assess pain characteristics regularly
- Rationale: Guide pain management
Administer prescribed pain medications
- Rationale: Provide comfort
Position patient for comfort
- Rationale: Minimize discomfort
Monitor pain response to interventions
- Rationale: Evaluate the effectiveness of the interventions.
Desired Outcomes:
- Pain reduction
- Improved comfort
- Enhanced rest
- Reduced anxiety
5. Knowledge Deficit
Nursing Diagnosis Statement:
Knowledge Deficit related to GI bleeding management evidenced by questions about self-care and prevention.
Related Factors/Causes:
- Limited exposure to the condition
- Complex medical terminology
- Anxiety about condition
- Multiple lifestyle modifications are needed
Nursing Interventions and Rationales:
Provide education about the condition
- Rationale: Enhance understanding
Teach warning signs
- Rationale: Enable early recognition
Review medication management
- Rationale: Ensure proper treatment
Discuss lifestyle modifications
- Rationale: Prevent recurrence
Desired Outcomes:
- Demonstrated understanding
- Proper medication compliance
- Recognition of warning signs
- Lifestyle modification adoption
Prevention and Patient Education
Medication Management
- Proper use of prescribed medications
- Avoidance of NSAIDs when contraindicated
- Anticoagulation monitoring
Lifestyle Modifications
- Smoking cessation
- Alcohol limitation
- Dietary adjustments
- Stress management
Warning Signs Recognition
- When to seek medical attention
- Symptoms of recurrent bleeding
- Emergency contact information
References
- Ackley, B. J., Ladwig, G. B., Makic, M. B., Martinez-Kratz, M. R., & Zanotti, M. (2023). Nursing diagnoses handbook: An evidence-based guide to planning care. St. Louis, MO: Elsevier.
- Antunes C, Tian C, Copelin II EL. Upper Gastrointestinal Bleeding. [Updated 2024 Aug 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470300/
- Harding, M. M., Kwong, J., & Hagler, D. (2022). Lewis’s Medical-Surgical Nursing: Assessment and Management of Clinical Problems, Single Volume. Elsevier.
- Herdman, T. H., Kamitsuru, S., & Lopes, C. (2024). NANDA International Nursing Diagnoses – Definitions and Classification, 2024-2026.
- Ignatavicius, D. D., Rebar, C., & Heimgartner, N. M. (2023). Medical-Surgical Nursing: Concepts for Clinical Judgment and Collaborative Care. Elsevier.
- Lau, J. Y. (2012). Evidence-based management of patients with acute non-variceal upper gastrointestinal bleeding. Gastrointestinal Intervention, 1(1), 53-57. https://doi.org/10.1016/j.gii.2012.09.002
- Orpen-Palmer J, Stanley AJ. Update on the management of upper gastrointestinal bleeding. BMJ Med. 2022 Sep 28;1(1):e000202. doi: 10.1136/bmjmed-2022-000202. PMID: 36936565; PMCID: PMC9951461.
- Silvestri, L. A. (2023). Saunders comprehensive review for the NCLEX-RN examination. St. Louis, MO: Elsevier.