Cellulitis is a common bacterial skin infection that affects the dermis and subcutaneous tissues. It usually occurs when bacteria such as Staphylococcus aureus or Streptococcus pyogenes enter through a break in the skin.
This condition can cause redness, swelling, warmth, and pain in the affected area.
For nurses, understanding the nursing diagnosis for cellulitis is essential for creating effective care plans, preventing complications, and ensuring patient recovery.
Pathophysiology
Cellulitis begins when bacteria invade through a skin break, triggering inflammation in the dermis and subcutaneous layers.
Vasodilation increases blood flow, leading to redness and warmth. Exudate accumulation causes swelling, and bacterial toxins stimulate pain receptors.
If untreated, infection may spread via the lymphatic or circulatory system, leading to sepsis or necrotizing fasciitis.
Nursing Assessment Cues
- Subjective data: Reports of pain, warmth, and tenderness in the affected area.
- Objective data: Erythema, swelling, edema, increased skin temperature, fever, chills, and possible lymphadenopathy.
- Diagnostics: Elevated WBC count, positive wound culture, and ultrasound (to rule out abscess).
- Risk factors: Diabetes, peripheral vascular disease, skin trauma, poor hygiene, and immunosuppression.
Nursing Care Plans for Cellulitis
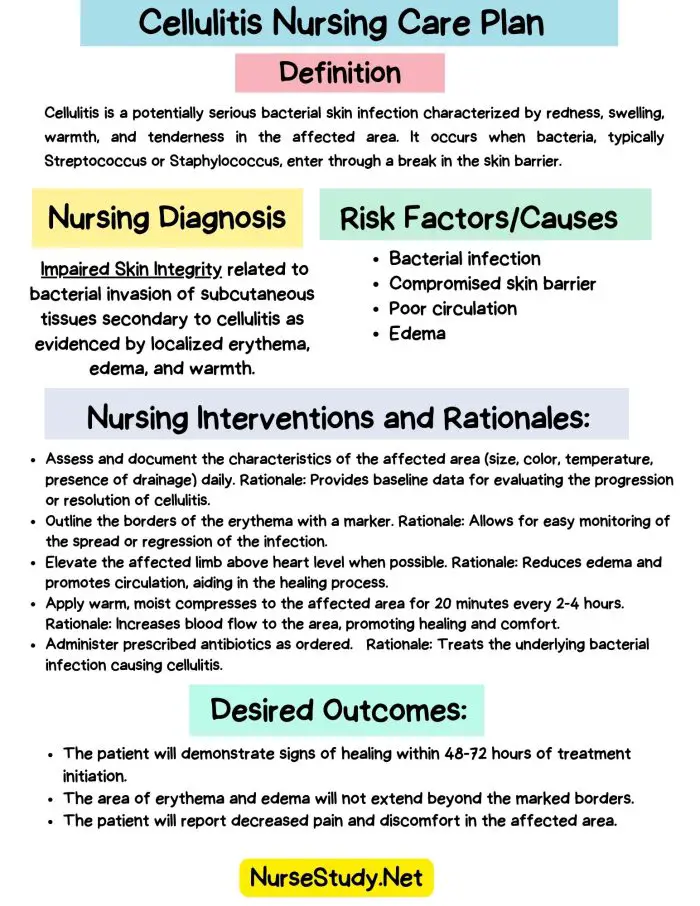
Nursing Care Plan #1 – Impaired Skin Integrity
Nursing Diagnosis Statement:
Impaired Skin Integrity related to disruption of skin surface secondary to cellulitis as evidenced by erythema, swelling, warmth, and open wound.
Related Factors:
- Bacterial invasion of skin tissue
- Inflammatory process
- Poor circulation or diabetes
Nursing Interventions and Rationales:
- Inspect and document wound characteristics daily to monitor healing progress and detect worsening infection.
- Apply prescribed topical antibiotics or dressings to promote healing and prevent reinfection.
- Maintain a clean and dry environment to reduce bacterial colonization.
- Elevate the affected extremity to decrease edema and promote venous return.
- Educate the patient on avoiding scratching or touching lesions to prevent secondary infection.
Desired Outcomes:
- Skin shows decreased redness and swelling.
- No new lesions appear.
- Patient verbalizes correct wound care techniques.
Nursing Care Plan #2 – Acute Pain
Nursing Diagnosis Statement:
Acute Pain related to the inflammatory process and tissue swelling secondary to cellulitis, as evidenced by the patient’s report of pain rated 7/10, facial grimacing, and guarding behavior.
Related Factors:
- Inflammation and tissue pressure
- Infection and edema
Nursing Interventions and Rationales:
- Assess pain level using a numeric scale to evaluate severity and treatment effectiveness.
- Administer prescribed analgesics or antipyretics to reduce pain and discomfort.
- Apply warm compresses (if ordered) to enhance circulation and relieve local discomfort.
- Encourage rest and proper limb elevation to reduce tissue pressure.
- Educate the patient on non-pharmacologic methods like relaxation or deep breathing.
Desired Outcomes:
- Pain score reduced to ≤3/10.
- Patient verbalizes comfort and effective coping strategies.
Nursing Care Plan #3 – Risk for Infection
Nursing Diagnosis Statement:
Risk for Infection related to open wound and impaired tissue defenses secondary to cellulitis.
Related Factors:
- Skin breakdown
- Invasive procedures or poor hygiene
Nursing Interventions and Rationales:
- Perform strict hand hygiene before and after wound care to prevent cross-contamination.
- Monitor for signs of systemic infection (fever, tachycardia, hypotension).
- Administer prescribed IV or oral antibiotics as ordered to eradicate infection.
- Educate the patient on completing the antibiotic course to prevent recurrence.
- Encourage adequate fluid intake to support immune function.
Desired Outcomes:
- No signs of spreading infection.
- Normal body temperature maintained.
- WBC count within normal limits.
Nursing Care Plan #4 – Ineffective Peripheral Tissue Perfusion
Nursing Diagnosis Statement:
Ineffective Peripheral Tissue Perfusion related to inflammatory swelling and impaired circulation as evidenced by edema, warmth, and delayed capillary refill.
Related Factors:
- Inflammation and edema compressing blood vessels
- Immobility or limb dependency
Nursing Interventions and Rationales:
- Assess peripheral pulses, skin color, and temperature to identify perfusion changes.
- Elevate affected limb above heart level to enhance venous return.
- Encourage ambulation or gentle exercises when possible to improve circulation.
- Avoid constrictive clothing or dressings that restrict blood flow.
- Monitor for complications like numbness or cyanosis.
Desired Outcomes:
- Improved capillary refill and skin temperature.
- Decrease in swelling and discomfort.
Nursing Care Plan #5 – Deficient Knowledge
Nursing Diagnosis Statement:
Deficient Knowledge related to lack of understanding about cellulitis management and prevention as evidenced by patient’s questions about wound care and antibiotic use.
Related Factors:
- Limited health literacy
- Inexperience with infection management
Nursing Interventions and Rationales:
- Explain the disease process and the importance of completing antibiotic therapy.
- Teach wound care techniques, including hand hygiene and dressing changes.
- Discuss prevention strategies (e.g., moisturizing dry skin, treating cuts promptly).
- Provide written materials for reinforcement.
- Encourage the patient to report recurrence signs like redness or fever early.
Desired Outcomes:
- The patient verbalizes understanding of the care plan and infection prevention.
- Demonstrates correct wound care technique.
Patient Education and Safety
- Complete the full antibiotic course even if symptoms improve.
- Keep the affected area clean and dry.
- Elevate the limb to reduce swelling.
- Report fever or spreading redness immediately.
FAQ
1. What is the priority nursing diagnosis for cellulitis?
Impaired skin integrity and risk for infection are top priorities due to the potential for sepsis.
2. What are the nursing interventions for cellulitis?
Monitor the wound, administer antibiotics, elevate the limb, manage pain, and educate the patient.
3. Can cellulitis recur?
Yes. Proper hygiene and skin protection can prevent recurrence.
4. Is cellulitis contagious?
No, but bacteria can spread through direct contact with wound drainage.
Peer-Reviewed References
- Brunner & Suddarth’s Textbook of Medical-Surgical Nursing (15th ed.)
- Lewis, Heitkemper, & Harding, Medical-Surgical Nursing: Assessment and Management of Clinical Problems (11th ed.)
- Ignatavicius & Workman, Medical-Surgical Nursing: Concepts for Interprofessional Collaborative Care (10th ed.)
- Gulanick & Myers, Nursing Care Plans: Diagnoses, Interventions, and Outcomes (10th ed.)
- Potter & Perry, Fundamentals of Nursing (10th ed.)