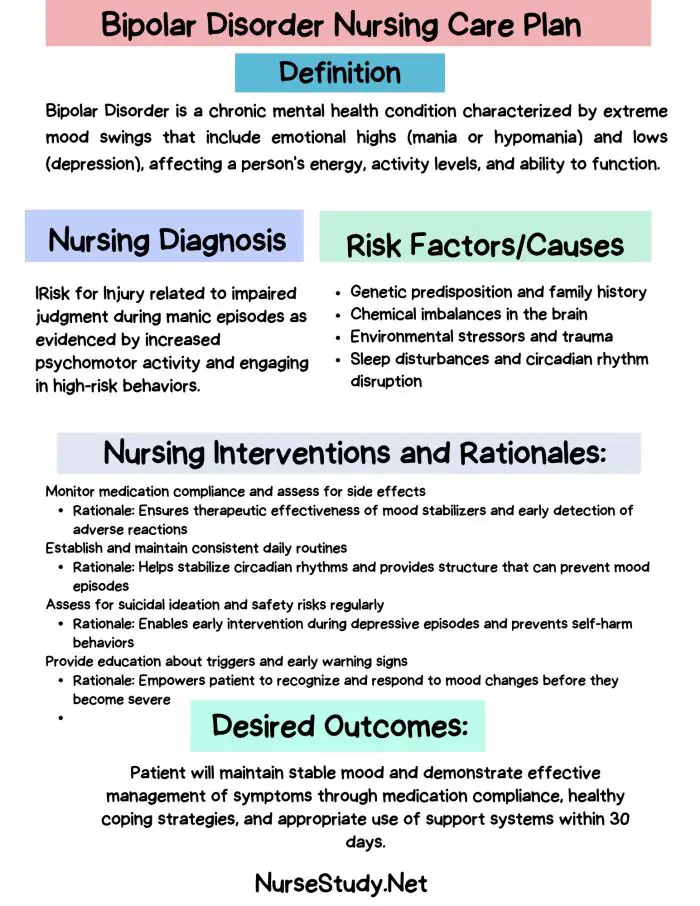
Bipolar disorder is a complex mental health condition characterized by extreme mood swings, ranging from manic highs to depressive lows.
As a psychiatric nurse, understanding and implementing effective Bipolar Disorder Nursing Diagnosis and care plan is crucial for providing optimal care to patients with bipolar disorder.
Understanding Bipolar Disorder
Bipolar disorder, formerly known as manic-depressive illness, is a chronic mental health condition that affects a person’s mood, energy levels, and ability to function in daily life. The disorder is characterized by alternating periods of mania (or hypomania) and depression, with potential periods of stability in between.
Manic Episodes
Manic episodes are characterized by:
- Elevated mood and increased energy
- Decreased need for sleep
- Racing thoughts and rapid speech
- Inflated self-esteem or grandiosity
- Increased goal-directed activity
- Engaging in risky or impulsive behaviors
Depressive Episodes
Depressive episodes involve:
- Persistent feelings of sadness or emptiness
- Loss of interest in previously enjoyed activities
- Changes in appetite and sleep patterns
- Fatigue and loss of energy
- Difficulty concentrating
- Feelings of worthlessness or guilt
- Thoughts of death or suicide
The Role of Psychiatric Nursing in Bipolar Disorder Management
Psychiatric nurses play a pivotal role in the care and management of patients with bipolar disorder. Their responsibilities include:
- Conducting comprehensive assessments
- Implementing and evaluating nursing interventions
- Administering and monitoring medication
- Providing psychoeducation to patients and families
- Collaborating with the interdisciplinary healthcare team
Effective nursing care for bipolar disorder patients revolves around creating and implementing tailored nursing care plans based on accurate nursing diagnoses.
Nursing Care Plans for Bipolar Disorder
The following section outlines five nursing care plans for patients with bipolar disorder. Each plan includes the nursing diagnosis statement, related factors, nursing interventions with rationales, and desired outcomes.
1. Risk for Suicide
Nursing Diagnosis Statement: Risk for Suicide related to depressive episodes of bipolar disorder, feelings of hopelessness, and previous suicide attempts.
Related Factors/Causes:
- Severe depressive symptoms
- History of suicide attempts
- Feelings of hopelessness and worthlessness
- Social isolation
- Impulsivity during manic episodes
Nursing Interventions and Rationales:
- Conduct frequent suicide risk assessments.
Rationale: Regular assessments help identify changes in suicidal ideation and allow for timely interventions. - Implement close observation protocols as per facility policy.
Rationale: Constant or frequent monitoring ensures patient safety and allows immediate intervention. - Remove potentially harmful objects from the patient’s environment.
Rationale: Eliminating access to means of self-harm reduces the risk of impulsive suicidal actions. - Engage the patient in developing a safety plan.
Rationale: Involving the patient in their safety planning promotes a sense of control and commitment to staying safe. - Administer prescribed medications and monitor for effectiveness and side effects.
Rationale: Proper medication management can help stabilize mood and reduce suicidal ideation.
Desired Outcomes:
- Patient will verbalize decreased suicidal ideation within 72 hours.
- The patient will demonstrate the use of coping strategies when experiencing suicidal thoughts.
- Patient will commit to a safety plan and contract for safety throughout hospitalization.
2. Disturbed Sleep Pattern
Nursing Diagnosis Statement: Disturbed Sleep Pattern related to a manic episode of bipolar disorder, as evidenced by decreased need for sleep and increased nighttime activity.
Related Factors/Causes:
- Manic or hypomanic state
- Racing thoughts
- Increased energy levels
- Circadian rhythm disruption
Nursing Interventions and Rationales:
- Establish a consistent sleep-wake schedule.
Rationale: Regular sleep patterns help regulate circadian rhythms and improve sleep quality. - Implement sleep hygiene practices (e.g., dim lighting, quiet environment).
Rationale: Creating a sleep-conducive environment promotes relaxation and facilitates sleep onset. - Limit caffeine and stimulating activities before bedtime.
Rationale: Reducing stimulants helps calm the mind and body, preparing for sleep. - Teach relaxation techniques such as deep breathing or progressive muscle relaxation.
Rationale: Relaxation exercises can help reduce racing thoughts and physical tension, promoting sleep. - Administer sleep medications as prescribed and monitor effectiveness.
Rationale: Pharmacological interventions may be necessary to establish a regular sleep pattern during acute manic episodes.
Desired Outcomes:
- Patient will demonstrate improved sleep patterns, achieving at least 6 hours of sleep per night within one week.
- The patient will report feeling more rested and less irritable during daytime hours.
- Patient will consistently use sleep hygiene practices and relaxation techniques to improve sleep quality.
3. Impaired Social Interaction
Nursing Diagnosis Statement: Impaired Social Interaction related to mood instability and inappropriate social behaviors, as evidenced by difficulty maintaining relationships and social withdrawal during depressive episodes.
Related Factors/Causes:
- Mood swings
- Impulsivity during manic episodes
- Social withdrawal during depressive episodes
- The stigma associated with bipolar disorder
Nursing Interventions and Rationales:
- Assess the patient’s current level of social functioning and support system.
Rationale: Understanding the patient’s baseline helps set realistic goals for improving social interaction. - Encourage participation in group therapy sessions.
Rationale: Group settings provide opportunities to practice social skills and receive peer support. - Teach and model appropriate social behaviors and communication skills.
Rationale: Improving social skills enhances the patient’s ability to form and maintain healthy relationships. - Facilitate family education and involvement in treatment.
Rationale: Family support and understanding can significantly improve social outcomes for patients with bipolar disorder. - Encourage participation in social activities within the treatment setting.
Rationale: Structured social interactions help build confidence and practice newly learned skills in a safe environment.
Desired Outcomes:
- Patient will demonstrate improved social interactions with staff and peers within two weeks.
- The patient will verbalize an understanding of how mood symptoms affect social relationships.
- Patient will actively participate in at least one group activity daily.
4. Ineffective Coping
Nursing Diagnosis Statement: Ineffective Coping related to mood instability and lack of effective coping mechanisms, as evidenced by substance abuse, impulsive behaviors, and difficulty managing stress.
Related Factors/Causes:
- Limited knowledge of effective coping strategies
- History of maladaptive coping mechanisms
- Overwhelming nature of bipolar symptoms
- Cognitive distortions associated with mood episodes
Nursing Interventions and Rationales:
- Assess current coping strategies and their effectiveness.
Rationale: Identifying existing coping mechanisms helps in building upon strengths and addressing weaknesses. - Teach and practice stress management techniques (e.g., mindfulness, progressive muscle relaxation).
Rationale: Equipping patients with effective stress management tools enhances their ability to cope with mood fluctuations. - Implement cognitive-behavioral therapy (CBT) techniques to address negative thought patterns.
Rationale: CBT helps patients recognize and modify unhelpful thoughts and behaviors, improving overall coping. - Encourage journaling or mood tracking.
Rationale: Self-monitoring helps patients identify triggers and patterns, facilitating proactive coping strategies. - Provide education on healthy lifestyle choices (e.g., exercise, nutrition, sleep hygiene).
Rationale: A healthy lifestyle supports mood stability and enhances overall coping abilities.
Desired Outcomes:
- The patient will demonstrate the use of at least two new coping strategies when faced with stressors within one week.
- The patient will verbalize understanding of the relationship between thoughts, feelings, and behaviors.
- Patient will report decreased use of maladaptive coping mechanisms (e.g., substance abuse, self-harm) throughout treatment.
5. Imbalanced Nutrition: Less Than Body Requirements
Nursing Diagnosis Statement: Imbalanced Nutrition: Less Than Body Requirements related to decreased appetite during depressive episodes, as evidenced by weight loss and inadequate food intake.
Related Factors/Causes:
- Depressive symptoms affecting appetite
- Side effects of medications
- Irregular eating patterns during mood episodes
- Neglect of self-care during severe mood states
Nursing Interventions and Rationales:
- Assess nutritional status, including weight, BMI, and recent dietary intake.
Rationale: Establishing a baseline helps monitor progress and tailor interventions. - Collaborate with a dietitian to develop an individualized meal plan.
Rationale: A personalized approach meets nutritional needs while considering patient preferences and medication effects. - Offer small, frequent meals and snacks throughout the day.
Rationale: Smaller portions may be more manageable for patients with decreased appetite. - Monitor and document food intake.
Rationale: Regular monitoring allows for timely interventions if nutritional goals are not being met. - Administer prescribed nutritional supplements if indicated.
Rationale: Supplements can help bridge nutritional gaps when dietary intake is insufficient.
Desired Outcomes:
- Patient will demonstrate a consistent pattern of adequate nutritional intake within two weeks.
- The patient will verbalize an understanding of the importance of proper nutrition in managing bipolar disorder.
- Patient will show stability or improvement in weight and nutritional status markers throughout treatment.
Conclusion
Effective nursing care for patients with bipolar disorder requires a comprehensive understanding of the condition, its symptoms, and the unique challenges it presents.
By implementing these nursing care plans, psychiatric nurses can provide targeted, evidence-based care that addresses the multifaceted needs of patients with bipolar disorder.
Regular assessment, individualized interventions, and ongoing evaluation are key to promoting stability, improving quality of life, and supporting long-term recovery for individuals living with bipolar disorder.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
- Berk, M., Post, R., Ratheesh, A., Gliddon, E., Singh, A., Vieta, E., … & Dodd, S. (2017). Staging in bipolar disorder: from theoretical framework to clinical utility. World Psychiatry, 16(3), 236-244.
- Culpepper, L. (2014). The diagnosis and treatment of bipolar disorder: decision-making in primary care. Primary Care Companion for CNS Disorders, 16(3).
- Geddes, J. R., & Miklowitz, D. J. (2013). Treatment of bipolar disorder. The Lancet, 381(9878), 1672-1682.
- Goodwin, G. M., Haddad, P. M., Ferrier, I. N., Aronson, J. K., Barnes, T. R. H., Cipriani, A., … & Young, A. H. (2016). Evidence-based guidelines for treating bipolar disorder: revised third edition recommendations from the British Association for Psychopharmacology. Journal of Psychopharmacology, 30(6), 495-553.
- National Institute for Health and Care Excellence. (2014). Bipolar disorder: assessment and management. NICE guideline [CG185].
- Townsend, M. C. (2015). Psychiatric mental health nursing: Concepts of care in evidence-based practice (8th ed.). Philadelphia, PA: F.A. Davis Company.
- Vieta, E., Berk, M., Schulze, T. G., Carvalho, A. F., Suppes, T., Calabrese, J. R., … & Grande, I. (2018). Bipolar disorders. Nature Reviews Disease Primers, 4(1), 1-16.