Tuberculosis is an infectious disease caused by Mycobacterium tuberculosis. It primarily affects the lungs but can also impact other organs.
TB spreads through airborne droplets when an infected person coughs, sneezes or speaks. While treatable and preventable, TB continues to be a significant health concern, especially in developing countries and among immunocompromised individuals.
There are three stages of TB infection:
- Exposure: Initial contact with an infected individual.
- Latent TB Infection (LTBI): The bacteria are present but dormant, with no active symptoms.
- Active TB Disease: The bacteria become active, causing symptoms and potential transmission to others.
Nursing Process for Tuberculosis
The nursing process for tuberculosis patients focuses on the following:
- Preventing disease transmission
- Ensuring adherence to long-term treatment regimens
- Managing symptoms and complications
- Providing patient and family education
Nurses play a crucial role in this process, from initial assessment to ongoing care and follow-up.
Nursing Assessment
Subjective Data Collection
- Chief Complaint: Note persistent cough (especially if lasting more than three weeks), chest pain, shortness of breath, fatigue, fever, night sweats, and unexplained weight loss.
- Health History:
- Previous TB exposure or diagnosis
- HIV status
- Immunosuppressive conditions or medications
- Recent travel to TB-endemic areas
- Substance abuse history
- Living or working conditions (crowded or poorly ventilated spaces)
- Family History: Any family members with TB diagnosis or symptoms
Objective Data Collection
- Physical Examination:
- Respiratory assessment: Rate, depth, use of accessory muscles, presence of dyspnea
- Lung auscultation: Crackles, wheezes, or decreased breath sounds
- Weight and nutritional status
- Presence of lymphadenopathy
- Diagnostic Tests:
- Tuberculin skin test (TST) or interferon-gamma release assay (IGRA)
- Chest X-ray
- Sputum culture and microscopy
- Complete blood count (CBC)
- Liver function tests
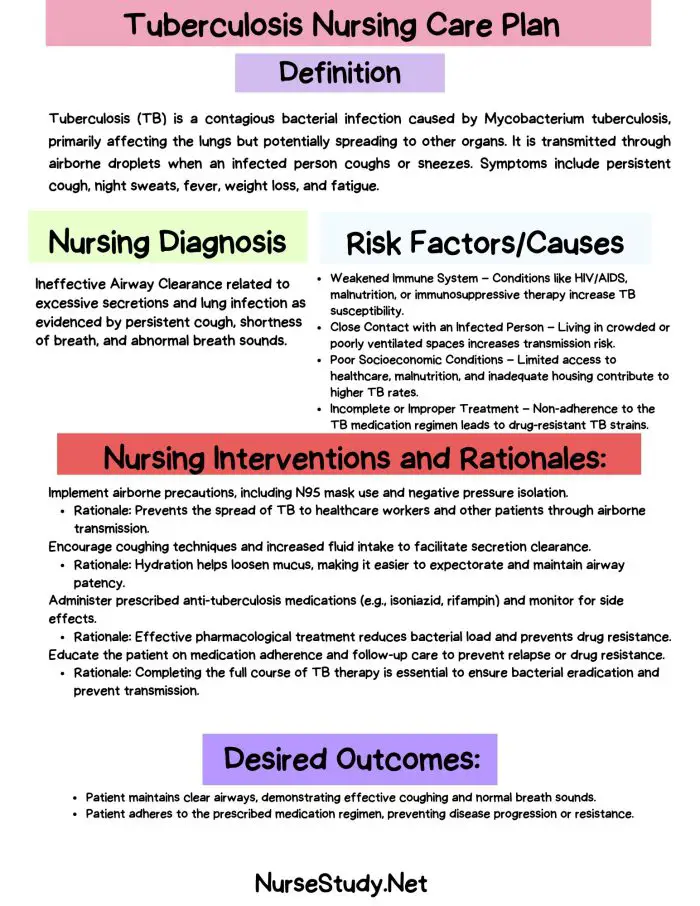
Nursing Diagnoses and Care Plans
Based on the assessment data, nurses can identify several potential nursing diagnoses for patients with tuberculosis. Here are five critical nursing diagnoses with their corresponding care plans:
1. Ineffective Breathing Pattern
Nursing Diagnosis: Ineffective Breathing Pattern related to inflammation and congestion of airways secondary to pulmonary tuberculosis, as evidenced by dyspnea, tachypnea, and use of accessory muscles.
Related Factors/Causes:
- Inflammation of lung tissue
- Accumulation of secretions
- Fatigue
- Anxiety
Nursing Interventions and Rationales:
- Assess respiratory rate, depth, and pattern every 4 hours. Rationale: Provides baseline data and helps detect early signs of respiratory distress.
- Position the patient in semi-Fowler’s or high Fowler’s position. Rationale: Promotes optimal lung expansion and eases breathing effort.
- Teach and encourage deep breathing and coughing exercises every 2 hours while awake. Rationale: Improves ventilation and helps mobilize secretions.
- Administer prescribed bronchodilators and monitor their effectiveness. Rationale: Helps relieve bronchospasm and improve air exchange.
- Provide oxygen therapy as prescribed and monitor oxygen saturation. Rationale: Ensures adequate oxygenation and prevents hypoxemia.
Desired Outcomes:
- Patient will demonstrate improved breathing pattern with respiratory rate within normal range (12-20 breaths/minute) and no use of accessory muscles.
- Patient will report decreased dyspnea and improved comfort in breathing.
2. Risk for Infection Transmission
Nursing Diagnosis: Risk for Infection Transmission related to active pulmonary tuberculosis and lack of knowledge about disease transmission.
Related Factors/Causes:
- Presence of Mycobacterium tuberculosis in sputum
- Inadequate knowledge of infection control measures
- Non-adherence to treatment regimen
Nursing Interventions and Rationales:
- Implement airborne precautions, including placing the patient in a negative pressure room. Rationale: Prevents the spread of TB bacteria through air currents.
- Educate the patient and family about proper cough etiquette and hand hygiene. Rationale: Reduces the risk of TB transmission through droplets and contact.
- Ensure all healthcare workers and visitors wear appropriate personal protective equipment (PPE), including N95 respirators. Rationale: Protects healthcare workers and visitors from inhaling infectious particles.
- Administer anti-tuberculosis medications as prescribed and monitor for adherence. Rationale: Effective treatment reduces bacterial load and infectivity.
- Teach the patient about the importance of completing the full course of treatment. Rationale: Prevents development of drug-resistant TB and reduces the risk of transmission.
Desired Outcomes:
- Patient will demonstrate understanding of infection control measures and consistently practice them.
- No new cases of TB will be linked to the patient during hospitalization or follow-up.
3. Imbalanced Nutrition: Less than Body Requirements
Nursing Diagnosis: Imbalanced Nutrition: Less than Body Requirements related to increased metabolic demands and decreased appetite secondary to tuberculosis infection, as evidenced by unintentional weight loss and reduced muscle mass.
Related Factors/Causes:
- Increased metabolic demands due to infection
- Decreased appetite
- Fatigue
- Nausea (potentially medication-induced)
Nursing Interventions and Rationales:
- Assess and document patient’s daily nutritional intake. Rationale: Provides baseline data to track nutritional status and guide interventions.
- Weigh the patient weekly and monitor for trends. Rationale: Weight is an objective measure of nutritional status and treatment effectiveness.
- Offer small, frequent, high-calorie, and high-protein meals. Rationale: Smaller meals may be better tolerated, while increased calories and protein support healing and immune function.
- Consult with a dietitian to develop an individualized nutrition plan. Rationale: Ensures nutritional needs are met while considering patient preferences and any dietary restrictions.
- Administer anti-nausea medications as prescribed before meals if needed. Rationale: Helps manage medication-induced nausea and improves food intake.
Desired Outcomes:
- Patient will demonstrate progressive weight gain towards goal weight.
- Patient will report improved appetite and increased energy levels.
4. Activity Intolerance
Nursing Diagnosis: Activity Intolerance related to an imbalance between oxygen supply and demand secondary to pulmonary tuberculosis, as evidenced by excessive fatigue and dyspnea upon exertion.
Related Factors/Causes:
- Decreased lung function
- Weakness
- Fatigue
- Malnutrition
Nursing Interventions and Rationales:
- Assess the patient’s activity tolerance using a standardized scale (e.g., Borg Scale). Rationale: Provides objective data to guide activity progression and monitor improvement.
- Implement a gradual activity progression plan, starting with simple activities of daily living. Rationale: Prevents overexertion while gradually improving stamina and strength.
- Teach energy conservation techniques, such as sitting while performing tasks when possible. Rationale: Helps the patient accomplish necessary activities without excessive fatigue.
- Collaborate with physical therapy for an individualized exercise plan. Rationale: Ensures safe and effective activity progression tailored to the patient’s condition.
- Monitor oxygen saturation before, during, and after activities. Rationale: Ensures adequate oxygenation and helps prevent respiratory distress during activities.
Desired Outcomes:
- The patient will report increased tolerance for daily activities without excessive fatigue or dyspnea.
- The patient will demonstrate gradual improvement in activity endurance as evidenced by increased duration and intensity of activities.
5. Deficient Knowledge
Nursing Diagnosis: Deficient Knowledge related to lack of exposure to information about tuberculosis management and prevention, as evidenced by verbalization of misconceptions and non-adherence to treatment plan.
Related Factors/Causes:
- Lack of exposure to TB education
- Misinterpretation of information
- Cognitive limitations
- Language or cultural barriers
Nursing Interventions and Rationales:
- Assess the patient’s current knowledge about TB, its treatment, and prevention methods. Rationale: Identifies knowledge gaps and misconceptions to guide education efforts.
- Provide education about TB transmission, treatment regimen, potential side effects of medications, and the importance of treatment adherence. Rationale: Increases patient’s understanding and promotes treatment adherence.
- Use teach-back method to confirm patient’s understanding of key points. Rationale: Ensures information is correctly understood and retained.
- Provide written materials in the patient’s preferred language and at an appropriate literacy level. Rationale: Reinforces verbal teaching and serves as a reference for the patient.
- Involve family members or support persons in education sessions when appropriate. Rationale: Enhances support system and improves adherence to treatment plan.
Desired Outcomes:
- The patient will verbalize an accurate understanding of tuberculosis, its treatment, and prevention methods.
- The patient will demonstrate adherence to the prescribed treatment regimen and follow-up appointments.
Prevention and Patient Education
Preventing the spread of tuberculosis and ensuring patient compliance with treatment are crucial aspects of TB management. Nurses play a vital role in educating patients and their families about:
- The importance of completing the entire course of antibiotic treatment
- Proper cough etiquette and respiratory hygiene
- The need for regular follow-up appointments and sputum tests
- Potential side effects of TB medications and when to seek medical attention
- The importance of notifying close contacts for TB screening
- Lifestyle modifications to support recovery (e.g., smoking cessation, nutrition)
Conclusion
Tuberculosis nursing diagnosis requires a comprehensive approach that addresses not only the physical symptoms but also the psychosocial aspects of the disease. By implementing these nursing diagnoses and care plans, nurses can provide high-quality, patient-centered care that promotes recovery and prevents disease transmission. Remember, early identification, proper assessment, and consistent follow-up are key to successful TB management.
References
- World Health Organization. (2023). Global Tuberculosis Report 2023. Retrieved from https://www.who.int/teams/global-tuberculosis-programme/tb-reports
- Centers for Disease Control and Prevention. (2023). Core Curriculum on Tuberculosis: What the Clinician Should Know.
- American Thoracic Society, CDC, and Infectious Diseases Society of America. (2022). Treatment of Drug-Susceptible Tuberculosis. Clinical Infectious Diseases, 63(7), e147-e195.
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2021). NANDA International Nursing Diagnoses: Definitions & Classification 2021-2023. Thieme.
- Carpenito, L. J. (2022). Nursing Diagnosis: Application to Clinical Practice (17th ed.). Wolters Kluwer.
- Scullion, J., & Holmes, S. (2022). Diagnosis and management of patients with tuberculosis. Nursing Standard, 37(3), 61-66.
- Zwerling, A., et al. (2023). Nursing Interventions to Improve Treatment Adherence among Patients with Drug-Resistant Tuberculosis: A Systematic Review. International Journal of Nursing Studies, 118, 103944.
- Doenges, M. E., Moorhouse, M. F., & Murr, A. C. (2022). Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions, and Rationales (15th ed.). F.A. Davis Company.