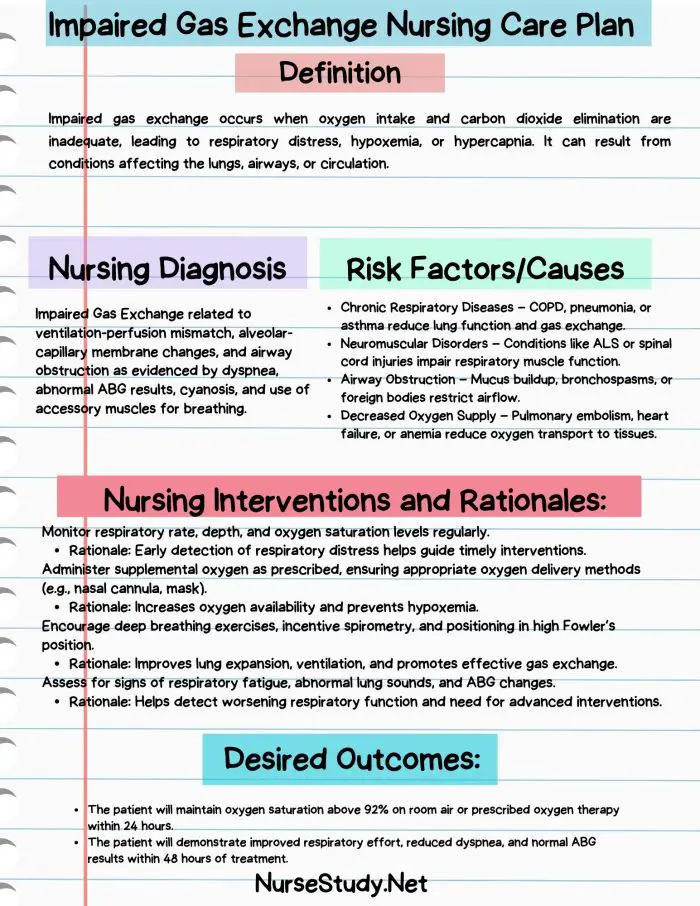
Impaired gas exchange is a critical nursing diagnosis that occurs when there’s a disruption in the normal exchange of oxygen and carbon dioxide between the lungs and the bloodstream.
This condition can seriously affect a patient’s overall health and requires prompt attention and intervention from healthcare providers.
Understanding Impaired Gas Exchange
Impaired gas exchange is often associated with other respiratory-related nursing diagnoses, such as ineffective breathing pattern or ineffective airway clearance. It can result from various physiological issues that affect the respiratory or circulatory systems, ultimately leading to inadequate oxygenation of tissues or ineffective removal of carbon dioxide from the body.
Causes (Related Factors)
Impaired gas exchange can stem from a wide range of conditions that affect the respiratory or circulatory systems. Some common causes include:
Respiratory disorders:
- Chronic Obstructive Pulmonary Disease (COPD)
- Asthma
- Pneumonia
- Pulmonary edema
- Acute Respiratory Distress Syndrome (ARDS)
Cardiovascular issues:
- Congestive heart failure
- Pulmonary embolism
- Congenital heart defects
Neurological conditions:
- Spinal cord injuries
- Neuromuscular disorders
Other factors:
- Obesity
- Smoking
- High altitude exposure
- Medication side effects (e.g., opioids causing respiratory depression)
Signs and Symptoms
Identifying impaired gas exchange requires a keen eye for subjective and objective symptoms. Here’s what to look out for:
Subjective Symptoms (Patient Reports)
- Shortness of breath (dyspnea)
- Chest pain or tightness
- Fatigue or weakness
- Dizziness or lightheadedness
- Confusion or difficulty concentrating
Objective Symptoms (Nurse Observes)
- Altered respiratory rate and pattern
- Use of accessory muscles for breathing
- Cyanosis (bluish discoloration of skin and mucous membranes)
- Restlessness or agitation
- Decreased level of consciousness
- Abnormal arterial blood gas (ABG) values
- Decreased oxygen saturation levels
- Tachycardia or bradycardia
- Hypotension or hypertension
Expected Outcomes
When developing a care plan for a patient with impaired gas exchange, nurses should aim for the following outcomes:
- The patient will demonstrate improved oxygenation, with oxygen saturation levels consistently above 95% (or as appropriate for their condition).
- The patient will report decreased shortness of breath and improved comfort level.
- The patient will maintain a respiratory rate within normal limits (12-20 breaths per minute for adults).
- The patient’s arterial blood gas values will return to or remain within normal ranges.
- The patient will demonstrate improved mental clarity and alertness.
- The patient can perform daily activities without excessive fatigue or respiratory distress.
Nursing Assessment
A thorough nursing assessment is crucial for identifying impaired gas exchange and developing an effective care plan. Here are key components of the assessment:
Review the patient’s medical history, focusing on respiratory and cardiovascular conditions.
Perform a comprehensive physical examination:
- Inspect the chest for symmetry and use of accessory muscles
- Auscultate lung sounds, noting any abnormalities such as wheezing, crackles, or diminished breath sounds
- Assess respiratory rate, depth, and pattern
- Check for cyanosis, particularly in the lips, nail beds, and mucous membranes
Monitor vital signs, including:
- Oxygen saturation levels using pulse oximetry
- Blood pressure
- Heart rate and rhythm
- Temperature
Evaluate the patient’s mental status and level of consciousness.
Review laboratory results:
- Arterial blood gas (ABG) analysis
- Complete blood count (CBC)
- Electrolyte levels
Assess the patient’s ability to perform activities of daily living and their energy levels.
Review current medications, particularly those that may affect respiratory function.
Evaluate the patient’s understanding of their condition and willingness to participate in treatment.
Nursing Interventions
Based on the assessment findings, nurses can implement various interventions to improve gas exchange:
Position the patient for optimal lung expansion:
- Elevate the head of the bed to 30-45 degrees
- Assist with frequent position changes
- Teach and encourage deep breathing and coughing exercises
Administer oxygen therapy as prescribed:
- Use appropriate delivery methods (nasal cannula, face mask, etc.)
- Monitor oxygen flow rate and adjust as needed
- Regularly assess the patient’s response to oxygen therapy
Maintain a patent airway:
- Suction secretions as needed
- Encourage the use of incentive spirometry
- Assist with chest physiotherapy if ordered
Administer prescribed medications:
- Bronchodilators
- Corticosteroids
- Antibiotics (if infection is present)
- Diuretics (for pulmonary edema)
Monitor and record fluid intake and output:
- Encourage adequate hydration to thin secretions
- Implement fluid restrictions if ordered for certain cardiac conditions
Provide patient education:
- Explain the importance of adherence to treatment plans
- Teach proper inhaler technique and use of other respiratory devices
- Discuss lifestyle modifications (e.g., smoking cessation, weight management)
Implement stress reduction techniques:
- Offer relaxation exercises
- Provide a calm environment
- Offer emotional support and reassurance
Collaborate with other healthcare professionals:
- Consult with respiratory therapists for specialized treatments
- Coordinate with physical therapists for mobility exercises
- Communicate with physicians regarding changes in patient status or need for treatment adjustments
Nursing Care Plans
Here are five detailed nursing care plans for patients with impaired gas exchange:
Care Plan 1: Impaired Gas Exchange related to COPD
Nursing Diagnosis Statement:
Impaired Gas Exchange related to alveolar-capillary membrane changes secondary to Chronic Obstructive Pulmonary Disease (COPD) as evidenced by dyspnea, use of accessory muscles, and oxygen saturation of 88% on room air.
Related Factors/Causes:
- Chronic inflammation of airways
- Destruction of alveolar walls
- Mucus hypersecretion
- Airflow limitation
Nursing Interventions and Rationales:
- Position the patient in a semi-Fowler’s or high Fowler’s position.
Rationale: Promotes lung expansion and eases breathing effort. - Administer oxygen therapy as prescribed, typically 1-2 L/min via nasal cannula.
Rationale: Improves oxygenation while avoiding CO2 retention risk in COPD patients. - Teach and assist with pursed-lip breathing and diaphragmatic breathing techniques.
Rationale: Helps control breathing rate and depth, reducing air trapping and improving gas exchange. - Administer bronchodilators as prescribed and monitor their effectiveness.
Rationale: Helps relax bronchial smooth muscles, improving airflow and gas exchange. - Encourage smoking cessation and provide resources if applicable.
Rationale: Smoking exacerbates COPD and further impairs gas exchange.
Desired Outcomes:
- The patient will maintain oxygen saturation ≥ 90% on prescribed oxygen therapy.
- The patient will demonstrate effective use of pursed-lip and diaphragmatic breathing techniques.
- The patient will report decreased dyspnea and improved ability to perform activities of daily living.
Care Plan 2: Impaired Gas Exchange related to Pneumonia
Nursing Diagnosis Statement:
Impaired Gas Exchange related to inflammation and edema of lung tissue secondary to pneumonia as evidenced by tachypnea, crackles on auscultation, and oxygen saturation of 91% on room air.
Related Factors/Causes:
- Alveolar inflammation
- Fluid accumulation in alveoli
- Decreased lung compliance
- Ventilation-perfusion mismatch
Nursing Interventions and Rationales:
- Assess respiratory rate, depth, and work of breathing every 2-4 hours.
Rationale: Early detection of respiratory distress allows for prompt intervention. - Auscultate lung sounds every 4 hours, noting the presence and location of crackles or other abnormal sounds.
Rationale: Helps track the progression or resolution of pneumonia. - Encourage deep breathing and coughing exercises every 2 hours while awake.
Rationale: Promotes airway clearance and improves ventilation. - Administer antibiotics as prescribed and monitor for side effects.
Rationale: Treats the underlying infection causing impaired gas exchange. - Provide oxygen therapy as ordered and monitor oxygen saturation levels.
Rationale: Supports oxygenation and prevents hypoxemia.
Desired Outcomes:
- The patient will demonstrate improved breath sounds with decreased crackles.
- The patient will maintain oxygen saturation ≥ 95% on room air or prescribed oxygen therapy.
- The patient will exhibit a respiratory rate within normal limits (12-20 breaths/minute for adults).
Care Plan 3: Impaired Gas Exchange related to Pulmonary Embolism
Nursing Diagnosis Statement:
Impaired Gas Exchange related to ventilation-perfusion mismatch secondary to pulmonary embolism as evidenced by sudden onset dyspnea, tachycardia, and decreased oxygen saturation of 89% on room air.
Related Factors/Causes:
- Obstruction of pulmonary blood flow
- Increased dead space ventilation
- Reflex bronchoconstriction
- Right ventricular strain
Nursing Interventions and Rationales:
- Monitor vital signs, including oxygen saturation, every 1-2 hours or as ordered.
Rationale: Allows for early detection of deterioration or improvement in patient’s condition. - Administer anticoagulation therapy as prescribed and monitor for bleeding.
Rationale: Prevents further clot formation and supports the dissolution of existing clots. - Position the patient in a semi-Fowler’s position or as comfortable.
Rationale: Reduces venous return to the heart and lungs, potentially easing breathing effort. - Provide oxygen therapy as ordered, titrating to maintain SpO2 ≥ 94%.
Rationale: Supports oxygenation and reduces strain on the right ventricle. - Assess for signs of anxiety or restlessness and provide reassurance.
Rationale: Anxiety can exacerbate dyspnea and tachycardia, further impairing gas exchange.
Desired Outcomes:
- The patient will maintain oxygen saturation ≥ 94% on prescribed oxygen therapy.
- The patient will report decreased dyspnea and chest pain.
- Patient will demonstrate stable vital signs, including heart rate < 100 bpm.
Care Plan 4: Impaired Gas Exchange related to Acute Respiratory Distress Syndrome (ARDS)
Nursing Diagnosis Statement:
Impaired Gas Exchange related to alveolar-capillary membrane damage secondary to Acute Respiratory Distress Syndrome (ARDS) as evidenced by severe hypoxemia (PaO2/FiO2 ratio < 200), bilateral infiltrates on chest X-ray, and use of mechanical ventilation.
Related Factors/Causes:
- Diffuse alveolar damage
- Pulmonary edema
- Decreased lung compliance
- Severe ventilation-perfusion mismatch
Nursing Interventions and Rationales:
- Implement lung-protective ventilation strategies as ordered (low tidal volumes, optimal PEEP).
Rationale: Minimizes further lung injury while supporting oxygenation and ventilation. - Perform frequent endotracheal suctioning using a closed suction system.
Rationale: Maintains airway patency while minimizing damage to alveoli. - Implement prone positioning as ordered, typically for 12-16 hours daily.
Rationale: Improves ventilation-perfusion matching and oxygenation in ARDS patients. - Monitor and record ventilator parameters, ABG results, and chest X-ray findings.
Rationale: Allows for assessment of treatment effectiveness and disease progression. - Administer sedation and neuromuscular blocking agents as prescribed.
Rationale: Facilitates ventilator synchrony and reduces oxygen consumption.
Desired Outcomes:
- The patient will demonstrate improved oxygenation with a PaO2/FiO2 ratio > 200.
- The patient will show clearing of bilateral infiltrates on chest X-ray.
- The patient will maintain stable hemodynamics during prone positioning.
Care Plan 5: Impaired Gas Exchange related to Neuromuscular Disorder
Nursing Diagnosis Statement:
Impaired Gas Exchange related to respiratory muscle weakness secondary to Guillain-Barré syndrome as evidenced by shallow breathing, decreased vital capacity, and arterial blood gas showing respiratory acidosis.
Related Factors/Causes:
- Progressive muscle weakness affecting respiratory muscles
- Inability to take deep breaths or cough effectively
- Risk of aspiration due to bulbar weakness
- Fatigue and increased work of breathing
Nursing Interventions and Rationales:
- Assess respiratory function regularly, including respiratory rate, depth, and use of accessory muscles.
Rationale: Allows for early detection of respiratory failure requiring ventilatory support. - Monitor vital capacity and negative inspiratory force measurements as ordered.
Rationale: These measurements can indicate the need for intubation and mechanical ventilation. - Assist with chest physiotherapy and incentive spirometry every 2-4 hours while awake.
Rationale: Helps maintain lung expansion and mobilize secretions. - Position the patient with the head elevated 30-45 degrees and frequently change position.
Rationale: Promotes optimal lung expansion and reduces the risk of aspiration. - Provide non-invasive ventilation (e.g., BiPAP) as prescribed, or prepare for intubation if needed.
Rationale: Supports respiratory function and prevents respiratory failure.
Desired Outcomes:
- The patient will maintain oxygen saturation ≥ 95% on room air or prescribed oxygen therapy.
- The patient will demonstrate stable or improving vital capacity measurements.
- The patient will exhibit no signs of respiratory distress or fatigue.
Conclusion
Impaired gas exchange is a severe nursing diagnosis that requires prompt recognition and intervention. By understanding the underlying causes, recognizing key signs and symptoms, and implementing appropriate nursing interventions, healthcare providers can significantly improve patient outcomes.
Regular assessment, timely interventions, and ongoing monitoring are crucial in effectively managing patients with impaired gas exchange.
Remember that each patient is unique, and care plans should be individualized based on specific patient needs, comorbidities, and responses to treatment. Collaboration with the interdisciplinary healthcare team is essential for comprehensive patient care and optimal outcomes.
References
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). NANDA International Nursing Diagnoses: Definitions & Classification 2018-2020. Thieme.
- Ackley, B. J., Ladwig, G. B., Makic, M. B. F., Martinez-Kratz, M., & Zanotti, M. (2020). Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care. Elsevier.
- Urden, L. D., Stacy, K. M., & Lough, M. E. (2018). Critical Care Nursing: Diagnosis and Management. Elsevier.
- Doenges, M. E., Moorhouse, M. F., & Murr, A. C. (2019). Nurse’s Pocket Guide: