Hyperglycemia, a condition characterized by elevated blood glucose levels, is a common health concern often associated with diabetes.
As a nurse, understanding hyperglycemia and developing appropriate nursing diagnoses is crucial for providing effective patient care.
What is Hyperglycemia?
Hyperglycemia occurs when blood glucose levels rise above normal ranges. Generally, fasting blood glucose levels above 125 mg/dL or postprandial (after-meal) levels exceeding 180 mg/dL are considered hyperglycemic.
Causes and Risk Factors
Several factors can contribute to hyperglycemia:
- Type 1 and Type 2 diabetes
- Endocrine disorders
- Pancreatic diseases
- Sedentary lifestyle
- Stress
- Medication side effects (e.g., corticosteroids)
- Illness or infection
- Excessive carbohydrate intake
Hyperglycemia Signs and Symptoms
Common symptoms of hyperglycemia include:
- Increased thirst (polydipsia)
- Frequent urination (polyuria)
- Increased hunger (polyphagia)
- Fatigue
- Blurred vision
- Headache
- Dry mouth
- Nausea
Complications
If left untreated, hyperglycemia can lead to serious complications:
- Cardiovascular disease
- Diabetic ketoacidosis (DKA)
- Hyperosmolar hyperglycemic state (HHS)
- Peripheral neuropathy
- Retinopathy
- Nephropathy
- Increased risk of infections
- Impaired wound healing
Nursing Process for Hyperglycemia
The nursing process is a systematic approach to patient care that includes assessment, diagnosis, planning, implementation, and evaluation. For patients with hyperglycemia, this process is crucial in managing blood glucose levels and preventing complications.
Assessment
- Obtain a thorough health history, including a family history of diabetes and other endocrine disorders.
- Assess current medications, particularly those that may affect blood glucose levels.
- Evaluate dietary habits and physical activity levels.
- Monitor blood glucose levels regularly.
- Assess for signs and symptoms of hyperglycemia.
- Perform a comprehensive physical examination, including neurological and vascular assessments.
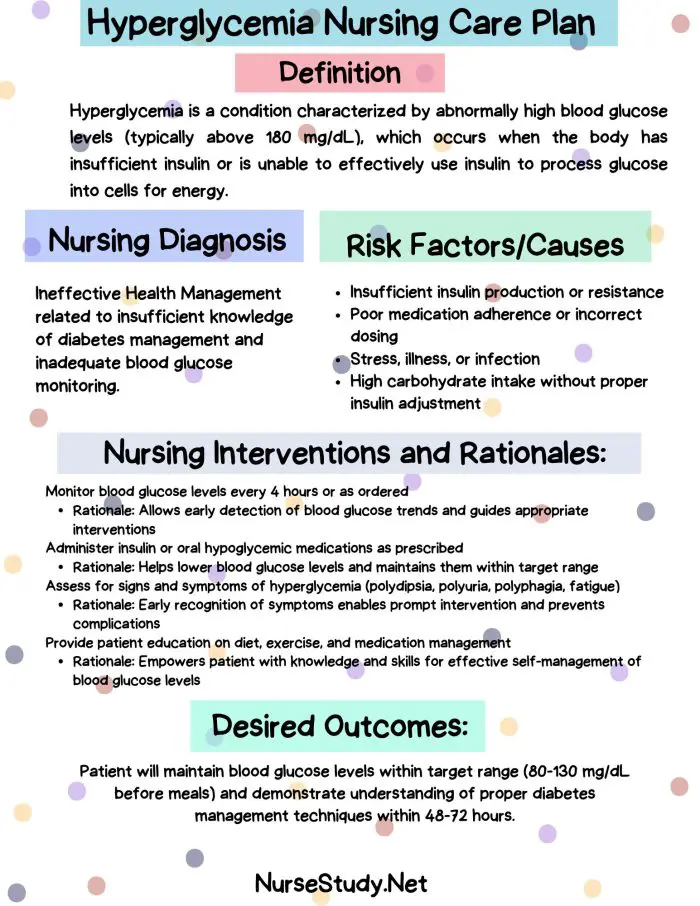
Nursing Diagnosis
Based on the assessment data, nurses can formulate appropriate nursing diagnoses. The following section provides detailed nursing care plans for common hyperglycemia nursing diagnoses.
Nursing Care Plans for Hyperglycemia
1. Ineffective Health Maintenance
Nursing Diagnosis Statement: Ineffective Health Maintenance related to insufficient knowledge about hyperglycemia management as evidenced by consistently elevated blood glucose levels and verbalized uncertainty about proper self-care techniques.
Related Factors/Causes:
- Lack of understanding about hyperglycemia and its management
- Inadequate resources or support systems
- Cultural or personal beliefs conflicting with health practices
- Cognitive or physical limitations affecting self-care abilities
Nursing Interventions and Rationales:
- Assess the patient’s current knowledge of hyperglycemia and its management.
Rationale: Identifies knowledge gaps and guides educational interventions. - Provide comprehensive education on hyperglycemia, including causes, symptoms, and management strategies.
Rationale: Empowers the patient with essential information for effective self-management. - Demonstrate and have the patient practice blood glucose monitoring techniques.
Rationale: Ensures accurate glucose monitoring and promotes patient independence. - Collaborate with a dietitian to develop a personalized meal plan.
Rationale: Helps manage carbohydrate intake and maintains optimal blood glucose levels. - Encourage regular physical activity and assist in developing an exercise plan.
Rationale: Physical activity improves insulin sensitivity and helps control blood glucose levels.
Desired Outcomes:
- The patient will demonstrate improved knowledge of hyperglycemia management as evidenced by an accurate verbal explanation of self-care techniques.
- The patient will maintain blood glucose levels within the target range, as evidenced by glucose logs.
- The patient will incorporate healthy lifestyle changes, including proper diet and regular exercise, into a daily routine.
2. Risk for Unstable Blood Glucose Levels
Nursing Diagnosis Statement: Risk for Unstable Blood Glucose Levels related to inadequate blood glucose monitoring and inconsistent medication adherence.
Related Factors/Causes:
- Insufficient knowledge about glucose monitoring
- Inconsistent medication regimen adherence
- Irregular meal patterns
- Stress or illness
- Lack of access to healthcare resources
Nursing Interventions and Rationales:
- Establish a consistent blood glucose monitoring schedule with the patient.
Rationale: Regular monitoring helps identify patterns and trends in glucose levels. - Educate the patient on the importance of medication adherence and proper administration techniques.
Rationale: Consistent medication use is crucial for maintaining stable blood glucose levels. - Assist the patient in developing a meal planning strategy that includes regular, balanced meals.
Rationale: Consistent meal patterns help stabilize blood glucose levels throughout the day. - Teach stress management techniques and the importance of maintaining routine during illness.
Rationale: Stress and disease can affect blood glucose levels; managing these factors promotes stability. - Connect the patient with community resources for ongoing diabetes management support.
Rationale: Continuous support and access to resources enhance long-term glycemic control.
Desired Outcomes:
- The patient will maintain blood glucose levels within the target range, as evidenced by glucose logs.
- The patient will demonstrate consistent adherence to the medication regimen as evidenced by self-report and medication logs.
- The patient will verbalize understanding of factors affecting blood glucose stability and strategies to manage them.
3. Deficient Knowledge
Nursing Diagnosis Statement: Deficient Knowledge related to lack of exposure to hyperglycemia management information as evidenced by verbalized misconceptions about diabetes care and inappropriate self-management behaviors.
Related Factors/Causes:
- Limited previous exposure to hyperglycemia education
- Misinterpretation of available information
- Cognitive limitations
- Language or cultural barriers
- Lack of interest in learning
Nursing Interventions and Rationales:
- Assess the patient’s learning style and preferences.
Rationale: Tailoring education to the patient’s learning style increases comprehension and retention. - Provide education on hyperglycemia, its causes, symptoms, and management using various teaching methods (verbal, written, visual).
Rationale: Multi-modal teaching approaches cater to different learning styles and reinforce key concepts. - Encourage the patient to ask questions and express concerns about their condition.
Rationale: Addressing patient concerns promotes engagement in the learning process and clarifies misunderstandings. - Use the teach-back method to confirm understanding of key concepts.
Rationale: This method helps identify areas needing further clarification and ensures accurate comprehension. - Provide culturally appropriate education materials in the patient’s preferred language.
Rationale: Culturally sensitive education improves patient engagement and understanding.
Desired Outcomes:
- The patient will demonstrate improved knowledge of hyperglycemia as evidenced by an accurate explanation of the condition and its management.
- The patient will correctly perform self-management tasks, including blood glucose monitoring and medication administration.
- The patient will identify reliable sources of diabetes information for ongoing learning.
4. Imbalanced Nutrition: More Than Body Requirements
Nursing Diagnosis Statement: Imbalanced Nutrition: More Than Body Requirements related to excessive caloric intake and sedentary lifestyle as evidenced by BMI >25 and elevated blood glucose levels.
Related Factors/Causes:
- Poor understanding of nutritional needs
- Cultural or personal food preferences high in calories and carbohydrates
- Sedentary lifestyle
- Emotional eating patterns
- Limited access to healthy food options
Nursing Interventions and Rationales:
- Collaborate with a dietitian to create an individualized meal plan.
Rationale: A personalized approach to nutrition supports weight management and glycemic control. - Educate the patient on portion control and healthy food choices.
Rationale: Understanding appropriate portions and nutritious options promotes balanced eating habits. - Teach carbohydrate counting techniques.
Rationale: Carbohydrate awareness helps manage blood glucose levels more effectively. - Encourage regular physical activity and assist in developing an exercise plan.
Rationale: Physical activity supports weight management and improves insulin sensitivity. - Address emotional eating patterns and teach stress management techniques.
Rationale: Managing emotional triggers for overeating supports long-term dietary adherence.
Desired Outcomes:
- The patient will demonstrate an understanding of proper nutrition for diabetes management, as evidenced by accurate meal planning.
- The patient will show gradual weight loss or maintain a healthy weight as appropriate.
- The patient will maintain blood glucose levels within the target range through proper nutrition and physical activity.
5. Risk for Infection
Nursing Diagnosis Statement: Risk for Infection related to elevated blood glucose levels and impaired immune function.
Related Factors/Causes:
- Hyperglycemia-induced impairment of white blood cell function
- Poor circulation, especially in extremities
- Frequent invasive procedures (e.g., blood glucose monitoring, insulin injections)
- Delayed wound healing
- Inadequate personal hygiene practices
Nursing Interventions and Rationales:
- Educate the patient on proper hand hygiene and overall hygiene practices.
Rationale: Good hygiene is crucial in preventing infections, especially in individuals with diabetes. - Teach proper techniques for blood glucose monitoring and insulin administration to minimize infection risk.
Rationale: Proper technique reduces the risk of introducing pathogens during these procedures. - Instruct on daily foot care and inspection.
Rationale: Regular foot care helps identify potential problems early and prevents diabetic foot complications. - Emphasize the importance of maintaining blood glucose within target ranges.
Rationale: Well-controlled blood glucose levels support immune function and reduce infection risk. - Educate on the signs and symptoms of infection and when to seek medical attention.
Rationale: Early recognition and treatment of infections is crucial in preventing serious complications.
Desired Outcomes:
- The patient will demonstrate proper hygiene practices, including hand washing and injection site care.
- The patient will maintain blood glucose levels within the target range.
- The patient will perform daily foot inspections and report any concerning findings promptly.
- The patient will remain free from infection as evidenced by the absence of signs and symptoms of infection.
Conclusion
Effective management of hyperglycemia requires a comprehensive nursing approach.
By implementing these nursing care plans, healthcare providers can help patients better understand and manage their condition, reducing the risk of complications and improving overall health outcomes.
References
- American Diabetes Association. (2021). Standards of Medical Care in Diabetes-2021. Diabetes Care, 44(Supplement 1), S1-S232.
- Doenges, M. E., Moorhouse, M. F., & Murr, A. C. (2019). Nursing Care Plans: Guidelines for Individualizing Client Care Across the Life Span. F.A. Davis Company.
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). NANDA International Nursing Diagnoses: Definitions & Classification 2018-2020. Thieme.
- Powers, M. A., Bardsley, J., Cypress, M., Duker, P., Funnell, M. M., Hess Fischl, A., … & Vivian, E. (2017). Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. The Diabetes Educator, 43(1), 40-53.
- Carpenito, L. J. (2017). Nursing diagnosis: Application to clinical practice. Wolters Kluwer.
- Dunning, T. (2019). Care of people with diabetes: A manual of nursing practice. John Wiley & Sons.
- Butcher, H. K., Bulechek, G. M., Dochterman, J. M. M., & Wagner, C. M. (2018). Nursing Interventions Classification (NIC)-E-Book. Elsevier Health Sciences.
- Moorhead, S., Johnson, M., Maas, M. L., & Swanson, E. (2018). Nursing Outcomes Classification (NOC)-E-Book: Measurement of Health Outcomes. Elsevier Health Sciences.