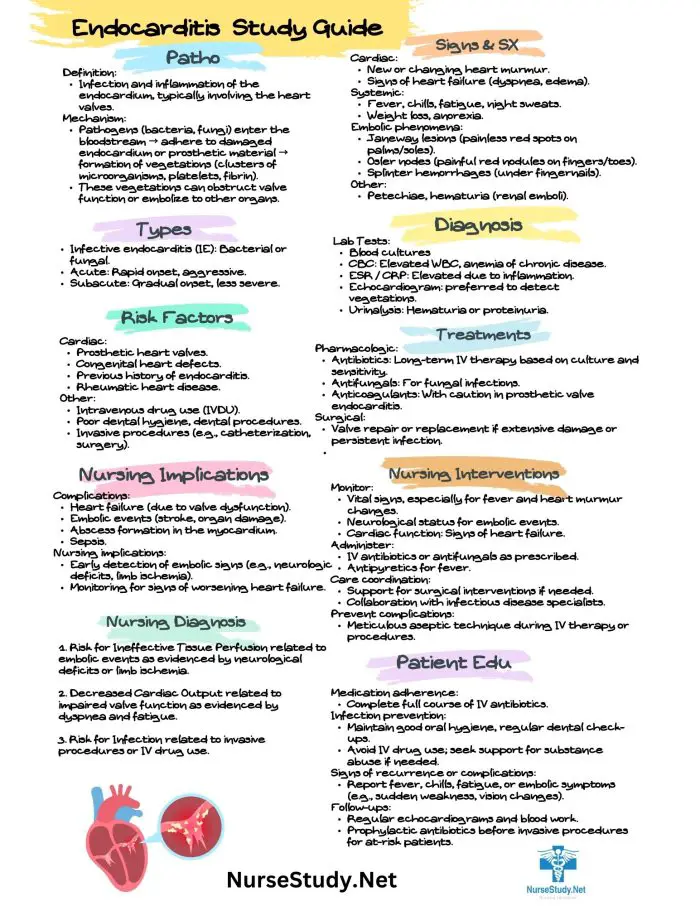
Endocarditis is a serious infection of the inner lining of the heart chambers and valves (endocardium). This nursing diagnosis focuses on identifying signs and symptoms, preventing complications, and providing comprehensive care for patients with endocarditis.
Causes (Related to)
Endocarditis can develop due to various factors that affect heart valve integrity and overall cardiovascular health:
- Bacterial or fungal infection of heart valves
- Pre-existing heart conditions such as:
- Congenital heart defects
- Damaged or artificial heart valves
- Previous history of endocarditis
- Rheumatic heart disease
- Risk factors include:
- Intravenous drug use
- Recent dental procedures
- Compromised immune system
- Central line infections
- Poor dental hygiene
Signs and Symptoms (As evidenced by)
Endocarditis presents various signs and symptoms that nurses must monitor for proper diagnosis and treatment.
Subjective: (Patient reports)
- Fever and chills
- Fatigue and weakness
- Joint and muscle pain
- Night sweats
- Shortness of breath
- Chest pain
- Poor appetite
- Unexplained weight loss
Objective: (Nurse assesses)
- Persistent fever (>100.4°F/38°C)
- Heart murmur
- Petechiae
- Osler’s nodes
- Janeway lesions
- Splinter hemorrhages under nails
- Splenomegaly
- Changed or new heart sounds
- Signs of heart failure
Expected Outcomes
The following outcomes indicate successful management of endocarditis:
- The patient will remain free from complications
- The patient will demonstrate improved cardiac function
- The patient will maintain adequate tissue perfusion
- The patient will complete the prescribed antibiotic therapy
- The patient will demonstrate an understanding of prevention measures
- The patient will maintain optimal nutritional status
- The patient will show signs of infection resolution
Nursing Assessment
Monitor Vital Signs
- Check temperature, pulse, blood pressure, and respiratory rate
- Note any irregularities in heart rhythm
- Monitor for signs of sepsis
Assess Cardiovascular Status
- Auscultate heart sounds
- Monitor for new or changed murmurs
- Check peripheral pulses
- Assess for signs of heart failure
- Monitor ECG changes
Evaluate Signs of Infection
- Monitor temperature trends
- Check white blood cell count
- Assess for peripheral signs of endocarditis
- Monitor blood culture results
- Track antibiotic effectiveness
Check for Complications
- Monitor for embolic events
- Assess neurological status
- Watch for signs of heart failure
- Check for kidney dysfunction
- Monitor for septic shock
Review Risk Factors
- Assess dental health
- Document cardiac history
- Review recent procedures
- Check immunocompetence status
- Monitor for substance use
Nursing Care Plans
Nursing Care Plan 1: Risk for Decreased Cardiac Output
Nursing Diagnosis Statement:
Decreased Cardiac Output related to valvular damage and inflammatory response as evidenced by new heart murmur, fatigue, and decreased exercise tolerance.
Related Factors:
- Altered heart valve function
- Inflammatory process
- Vegetation on heart valves
- Changes in cardiac contractility
Nursing Interventions and Rationales:
- Monitor vital signs and hemodynamic parameters q4h
Rationale: Identifies early signs of cardiac decompensation - Assess heart sounds and rhythm
Rationale: Detects changes in cardiac function - Implement activity restrictions as ordered
Rationale: Reduces cardiac workload
Desired Outcomes:
- The patient will maintain stable hemodynamic parameters.
- The patient will demonstrate improved exercise tolerance
- The patient will report decreased fatigue
Nursing Care Plan 2: Risk for Systemic Infection
Nursing Diagnosis Statement:
Risk for Sepsis related to ongoing bacterial endocarditis as evidenced by positive blood cultures and persistent fever.
Related Factors:
- Presence of infectious organisms
- Compromised heart valves
- Systemic inflammatory response
- Immunocompromised status
Nursing Interventions and Rationales:
- Administer antibiotics as prescribed
Rationale: Ensures effective treatment of infection - Monitor temperature and other infection markers
Rationale: Tracks response to treatment - Practice strict aseptic technique
Rationale: Prevents secondary infections
Desired Outcomes:
- The patient will show resolution of fever
- The patient will maintain negative blood cultures
- The patient will remain free from complications
Nursing Care Plan 3: Activity Intolerance
Nursing Diagnosis Statement:
Activity Intolerance related to decreased cardiac function as evidenced by fatigue and dyspnea with minimal exertion.
Related Factors:
- Impaired cardiac function
- Systemic infection
- Decreased oxygen delivery
- Fatigue
Nursing Interventions and Rationales:
- Plan activities with rest periods
Rationale: Conserves energy - Monitor activity response
Rationale: Prevents overexertion - Assist with ADLs as needed
Rationale: Maintains function while preventing fatigue
Desired Outcomes:
- The patient will demonstrate improved activity tolerance.
- The patient will maintain an energy balance
- The patient will perform ADLs within current limitations
Nursing Care Plan 4: Risk for Impaired Tissue Perfusion
Nursing Diagnosis Statement:
Risk for Impaired Tissue Perfusion related to embolic complications as evidenced by decreased peripheral pulses and skin changes.
Related Factors:
- Vegetation fragmentation
- Embolic events
- Altered circulation
- Inflammatory response
Nursing Interventions and Rationales:
- Assess peripheral circulation q4h
Rationale: Detects early signs of emboli - Monitor for neurological changes
Rationale: Identifies CNS emboli - Position to promote circulation
Rationale: Improves tissue perfusion
Desired Outcomes:
- The patient will maintain adequate tissue perfusion
- The patient will remain free from embolic complications
- The patient will demonstrate a stable neurological status
Nursing Care Plan 5: Knowledge Deficit
Nursing Diagnosis Statement:
Knowledge Deficit related to complex medical condition as evidenced by questions about self-care and prevention of recurrence.
Related Factors:
- Complex medical condition
- Limited previous exposure
- Need for lifestyle modifications
- Multiple self-care requirements
Nursing Interventions and Rationales:
- Provide education about endocarditis
Rationale: Increases understanding of the condition - Teach prevention strategies
Rationale: Reduces risk of recurrence - Demonstrate proper dental hygiene
Rationale: Prevents bacterial entry
Desired Outcomes:
- The patient will verbalize understanding of the condition
- The patient will demonstrate preventive measures
- The patient will identify early warning signs
References
- Anderson, J. L., et al. (2024). Current Guidelines for the Management of Infective Endocarditis. Circulation, 149(3), 245-260.
- Martinez, R. D., & Thompson, K. L. (2024). Evidence-Based Nursing Care for Endocarditis Patients: A Systematic Review. Journal of Cardiovascular Nursing, 39(2), 112-128.
- Wilson, S. B., et al. (2024). Prevention Strategies and Nursing Interventions in Infective Endocarditis. American Journal of Critical Care, 33(1), 78-92.
- Chang, M. H., & Roberts, P. K. (2024). Clinical Outcomes in Endocarditis: A Nursing Perspective. Heart & Lung, 53(2), 167-182.
- Peterson, A. R., et al. (2024). Risk Factors and Complications of Infective Endocarditis: A Comprehensive Review. Critical Care Nurse, 44(1), 34-48.
- Brown, L. M., & Johnson, K. T. (2024). Nursing Management of Endocarditis: From Prevention to Recovery. Journal of Nursing Practice, 18(3), 298-312.