Last updated on February 20th, 2023 at 09:15 am
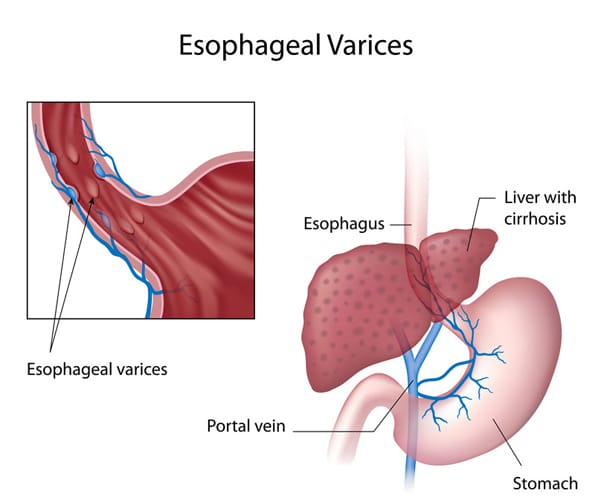
Esophageal varices are veins that are abnormally enlarged and are usually found on the lower two-thirds of the esophagus.
They arise from the blockage of the portal vein of the liver. Instead of flowing through the portal vein, the blood flows through the smaller blood vessels, which eventually causes venous enlargement, leakage, or even rupture.
The treatment plan for esophageal varices is mainly focused on the prevention or stoppage of their rupture and bleeding.
Signs and Symptoms of Esophageal Varices
Unless they are bleeding, esophageal varices may not present any signs or symptoms. A patient with bleeding esophageal varices may show:
- Hematemesis or vomiting large amounts of blood
- Black, tarry or bloody stools
- Dizziness
- Lightheadedness
- Loss of consciousness due to severe bleeding
Esophageal varices related to liver disease may have the following symptoms:
- Jaundice or yellow coloration of eyes and skin
- Ascites or abdominal fluid buildup
- Getting easily bruised
Causes and Risk Factors of Esophageal Varices
Liver disease cause scarring of the liver tissue known as cirrhosis of the liver. The liver scar tissues facilitate the backing up of the blood flow, thus increasing the pressure in the liver’s portal vein.
This condition is known as portal hypertension. To compensation for the increased pressure, the blood is forced to flow in smaller veins, including those veins that are found in the esophagus’ lowest part.
Their small size means that they cannot accommodate a large volume of blood. The veins may balloon, rupture, and bleed in time.
Aside from liver cirrhosis, thrombosis or the formation of blood clot in the portal vein or splenic vein may cause esophageal varices.
Parasitic infection of the liver, such as schistosomiasis found in Asia, Africa, Caribbean countries, and South America, can cause liver damage and lead to the formation of esophageal varices.
Alcohol abuse may lead to the rupture and bleeding of esophageal varices.
Complications of Esophageal Varices
Bleeding is the most life-threatening complication of esophageal varices. Internal bleeding may result to shock due to loss of a significant amount of blood, and this is fatal.
Another complication of esophageal varices is the increased risk for another rupture and bleeding episode of other varices.
Diagnosis of Esophageal Varices
- Physical examination and history taking – to check for any hematemesis, black tarry or blood stools, as well as to explore any alcohol abuse or history of liver disease
- Endoscopy – to visualize the gastrointestinal system, looking for any dilation of veins and any presence of red spots or red streaks which may indicate a very high risk of rupture and bleeding. Treatment of bleeding esophageal varices can also be done during this exam.
- Capsule endoscopy – to perform endoscopy but with the use of a capsule that has a camera in it. The patient swallows this like a pill, and the camera takes images of the GI tract as it goes down. This is more expensive than the usual endoscopy, but can be helpful for those who cannot tolerate the endoscope tube
- Imaging – CT scan and ultrasound Doppler of the portal and splenic veins
Treatment of Esophageal Varices
- Portal vein drugs. Beta blockers such as propanolol and nadolol can help treat portal hypertension by lowering the blood pressure in the portal vein. These reduce the risk for esophageal varices rupture and bleeding. After a bleeding episode, drugs like vasopressin and octreotide can be prescribed for up to 5 days to reduce the blood flow in the portal vein.
- Endoscopic band ligation. This procedure can be done while the patient is undergoing endoscopic exam and the doctor finds out that there are esophageal varices that are bleeding, or at high risk of rupture and bleed in the future. The doctor uses an elastic band to tie off the veins that are bleeding.
- Balloon tamponade. To stop the bleeding, this procedure involves inflating a balloon temporarily (for up to 24 hours) in order to place pressure on the esophageal varices.
- Transjugular intrahepatic portosystemic shunt (TIPS). This procedure is used to create a diversion of the blood flow away from the portal vein by means of making a shunt or an opening between the hepatic vein and the portal vein.
Esophageal Varices Nursing Diagnosis
Nursing Care Plan for Esophageal Varices 1
Nursing Diagnosis: Risk for Bleeding secondary to esophageal varices
Desired Outcome: The patient will be able to avoid having any frank or occult bleeding and will remain hemodynamically stable.
| Esophageal Varices Nursing Interventions | Rationales |
| Assess vital signs and observe for any signs of bleeding such as melena (black, tarry or bloody stools) and hematemesis (vomiting of blood). | To check for any signs of rupture and bleeding of esophageal varices. Hypotension, tachypnea, and tachycardia may indicate internal bleeding or hemorrhage. |
| Perform a focused assessment on the abdominal region, particularly checking for ascites. | Ascites is one of the symptoms of esophageal varices. This can manifest as distended abdomen, feeling of fullness, and rapid weight gain. |
| Administer drugs that can reduce portal hypertension, as prescribed. | Medications such as propanolol and nadolol are called beta blockers, and they can help treat portal hypertension by lowering the blood pressure in the portal vein. This reduces the risk for esophageal varices rupture and bleeding. |
| Explain what endoscopic band ligation means, its risks and its benefits. Prepare the patient for the procedure. | To inform the patient, gain consent for the procedure, and prepare the patient physically and mentally towards the intervention. Endoscopic band ligation can reduce the risk of rupture and bleed in the future. The doctor uses an elastic band to tie off the veins that are bleeding. |
Nursing Care Plan for Esophageal Varices 2
Nursing Diagnosis: Imbalanced Nutrition: Less than Body Requirements related to digestive tract bleeding secondary to esophageal varices, as evidenced by hematemesis, weight loss, nausea and vomiting, loss of appetite and dizziness/ lightheadedness
Desired Outcome: The patient will be able to achieve a weight within his/her normal BMI range, demonstrating healthy eating patterns and choices.
| Esophageal Varices Nursing Interventions | Rationale |
| Explore the patient’s daily nutritional intake and food habits (e.g. meal times, duration of each meal session, snacking, etc.) | To create a baseline of the patient’s nutritional status and preferences. |
| Create a daily weight chart and a food and fluid chart. Discuss with the patient the short term and long-term nutrition and weight goals related to peptic ulcer disease. | To effectively monitory the patient’s daily nutritional intake and progress in weight goals. |
| Help the patient to select appropriate dietary choices and limit alcohol intake. | To promote ulcer healing and healthy food habits. Alcohol abuse can cause liver cirrhosis, which can eventually lead to portal hypertension and formation of esophageal varices. |
| Refer the patient to the dietitian. | To provide a more specialized care for the patient in terms of nutrition and diet in relation to newly diagnosed disease. |
| Encourage soft foods such as bananas and yogurts. | To reduce irritation of the esophagus and ensure that the patient receives the right amount of nutrition. |
Nursing Care Plan for Esophageal Varices 3
Risk for Decreased Cardiac Output
Nursing Diagnosis: Risk for Decreased Cardiac Output related to bleeding secondary to esophageal varices.
Desired Outcomes:
- The patient will exhibit adequate cardiac output after the bleeding is controlled as evidenced by stable vital signs, normal peripheral perfusion, adequate intake and output, warm and dry skin, absence of breathing difficulties, and normal level of consciousness.
- The patient will be able to demonstrate self-care activities to improve gastrointestinal and cardiac health.
Nursing Care Plan for Esophageal Varices 4
Risk for Deficient Fluid Volume
Nursing Diagnosis: Risk for Deficient Fluid Volume related to nausea and hematemesis secondary to esophageal varices.
Desired Outcomes:
- The patient will verbalize a decrease in the severity of nausea and vomiting.
- The patient will maintain adequate fluid volume while waiting for treatment as evidenced by stable vital signs, adequate skin perfusion, strong peripheral pulses, alert mental state, and urine output greater than 30ml per hour.
| Esophageal Varices Nursing Interventions | Rationale |
| Assess and monitor the patient’s vital signs and mental status. Check for orthostatic changes, capillary refill, central and peripheral pulses, and abnormal heart rhythms through ECG. | One of the common signs of fluid loss from excessive vomiting or hematemesis is orthostatic hypotension. Capillary refill time is a quick measurement of intravascular volume. Pulses may become weak and low during fluid loss. Abnormal heart rhythms may occur due to electrolyte imbalance and fluid loss. |
| Assess and monitor the patient’s skin turgidity, respiratory status, and mental status. Check the skin and mucous membranes, level of consciousness, and blood oxygen level using pulse oximetry. | Dry skin and mucous membranes are early signs of dehydration. Pulse oximetry can detect adjustments in blood oxygen levels. Restlessness and anxiety can be early signs of hypovolemia while confusion and loss of consciousness are late signs. |
| Assess and record the characteristic, frequency, and amount of hematemesis. Check for nausea and melena or black tarry stool Measure and record the patient’s weight, intake, and output. | This will help the nurse detect increased bleeding, ulceration, and/or rupture of esophageal varices. Weight loss and decreased urine output may signify a decreased circulatory blood volume from the hematemesis and bleeding. |
| Check for coughing or choking signs. | Coughing or choking are the hallmark signs of hematemesis or bleeding esophageal varices. |
| Check and monitor the patient’s laboratory values such as electrolyte levels, CBC, CMP, INR or PT, ABGs, occult blood, and urine test. | Patients with esophageal varices may have metabolic acidosis from the excessive fluid loss, elevated WBC, BUN, creatinine, sodium, potassium, ammonia, lactate, ALT, AST; low hemoglobin, hematocrit, and platelet; elevated INR or prolonged PT, occult blood, and high urine specific gravity. |
| Place the patient in a semi- or high-Fowler’s position. Provide a comfortable and quiet environment with minimal stimulus. | This will help the patient in the expulsion of hematemesis, to suction excess secretions, and prevent aspiration during acute episodes of vomiting. A comfortable and quiet environment helps the patient get adequate rest, conserve energy, and prevent triggers of nausea and vomiting. |
| Educate the patient about the NPO status as ordered. Provide an emesis basis at the patient’s bedside. | This will help the patient’s stomach to rest and prevent vomiting from the foods being introduced. Emesis basis must be placed in an area where the patient can easily reach in cases of acute episodes of vomiting. |
| Encourage and provide frequent oral care as needed. | This will help decrease the unpleasant taste and odors in the mouth from the frequent vomiting. |
| Insert an IV line and administer fluids such as isotonic or colloid solutions as ordered. | This will help maintain adequate blood volume and urine output, and correct fluid and electrolyte imbalances. |
| Insert a nasogastric tube as ordered. | An NGT will help in the assessment of the severity of bleeding, gastric lavage, medication administration, and slow introduction of foods after acute episodes of vomiting. |
| Administer antiemetics as ordered. | This will prevent nausea and treat vomiting. |
| Prepare the patient for a procedure such as an endoscopy, ultrasound, and computed tomography scan as indicated. | These procedures will assist the healthcare team in identifying the cause of vomiting and bleeding. |
| Encourage nonpharmacological and diversional activities such as deep breathing exercises, diaphragmatic breathing, relaxation, guided imagery, distraction, or music therapy. | These techniques can help the patient relieve anxiety, thereby reducing metabolic rate and cardiac and respiratory workload. |
| Educate the patient about the slow introduction of food as tolerated. Starting with ice chips or ginger products dry food like crackers to bland diets like gelatine given in frequent small amounts. | After acute episodes of vomiting, a slow introduction of foods can help relieve nausea and maintain nutritional status. |
| Educate the patient and significant others about fluid and dietary options along with prescribed medications. | Adequate information can help in promoting adequate hydration, nutritional status, and compliance with the treatment plan. |
| Educate the patient and significant others about the condition, signs and symptoms to watch out for, and the interventions needed. | Giving adequate information can help prevent the progression and development of complications. |
Nursing Care Plan for Esophageal Varices 5
Nursing Diagnosis: Risk for Injury related to lightheadedness secondary to bleeding esophageal varices.
Desired Outcomes:
- The patient will be able to prevent injury by exercising fall prevention protocols.
- The patient will be able to prevent injury by doing activities within the parameters of limitation and modifying the environment to adapt to the patient’s capacity.
- The patient will be able to perform activities of daily living with minimal supervision and maintain a treatment regimen to regain balance and increase compliance.
| Esophageal Varices Nursing Interventions | Rationale |
| Assess and monitor the patient’s vital signs and mental status. Check for orthostatic changes, capillary refill, central and peripheral pulses, level of consciousness, and blood oxygen level using pulse oximetry. | A decrease in circulating blood volume may cause lightheadedness or orthostatic hypotension and may result in falls. Checking the pulses, capillary refill time, and blood oxygen levels may help in the early detection of decreased intravascular volume and cerebral perfusion. |
| Assess the patient’s functional level of mobility using the Bedside Mobility Assessment Tool (BMAT) which includes: Level 1: Sit and shake (repositioning, turning, and limb holding) Level 2: Stretch (extending the leg, straightening the knee, dorsiflexion, and plantar flexion) Level 3: Stand (ask the patient to seat, then to stand upright for up to 1 minute) Level 4: Step (marching in place and moving forward) | Bedside Mobility Assessment Tool (BMAT) is a simple tool used to assess functional mobility status and select appropriate equipment to safely mobilize the patient. |
| Assess the patient’s ability to perform Activities of Daily Living (ADLs) safely and efficiently using the following scale: 0 – Total independence 1 – Requires use of devices or equipment 2 – Requires assistance, instruction, and supervision 3 – Requires assistance from another person and/or equipment device 4 – Dependent on others or does not engage in any activity | Checking the patient’s functional level to perform activities of daily living will help the nurse plan activities based on the patient’s tolerance. |
| Provide a safe environment by raising bedside rails, lowering the bed, and keeping important items within reach. Assess the patient’s environment for any hazards, blockages, or obstacles. | These measures reduce the risk of falls due to the patient’s lightheadedness. Ensuring the safety of the environment before performing any activities must be a priority to prevent accidents and injury. |
| Elevate the lower extremities and place a pillow under the knees assuming a comfortable position. Use compression stockings and routinely turn the patient. | Elevating the lower extremities, using compression stockings, and frequent turning of the patient promote cerebral perfusion and venous return to the systemic circulation. |
| Assist the patient in performing passive ROM exercises in all extremities. Gradually introduce active ROM as tolerated. | These exercises increased systemic venous return preventing lightheadedness. |
| Assist the patient in ambulation as tolerated. Instruct the patient to sit down on the side of the bed, then slowly dangle the legs on the side of the bed, asking the patient to stand up for a few minutes before walking slowly. | Gradual position changes are done to dizziness from sudden changes in blood pressure or orthostatic hypotension. |
| Insert an IV line and administer fluids such as isotonic or colloid solutions as ordered. | This will help maintain adequate blood volume in circulation and adequate perfusion. |
| Assist the patient with activities of daily living as tolerated. Encourage independent activities without any deadline for accomplishment. Discontinue the activity if the patient presents with dizziness, lightheadedness, headache, syncope, etc, and notify the physician immediately. | This will promote confidence and independence to complete the patient’s daily routine without risking the patient’s safety. Spontaneous movements can cause dizziness, letting the patient accomplish the task at his/her own pace. The following signs and symptoms are due to decreased tissue oxygenation from overexertion. |
| Educate the patient about the use of mobility devices such as canes, walkers, crutches, etc. inform the significant others about proper transfer methods when assisting, moving, and transferring the patient to bed, chair, or stretcher. | These devices and methods aid in mobility, promote safety and activity tolerance, conserve energy, and support balance if the patient suddenly develops light-headedness. |
| Educate the patient about energy conservation techniques such as pushing rather than pulling, sliding rather than lifting, and placing items within reach. | Exhaustion can cause light-headedness, this energy-saving technique should be done to prevent exhaustion from daily activities. |
| Provide rest periods in between activities. Provide a quiet and comfortable environment for rest. | A good rest especially at night helps the patient regain adequate energy to accomplish activities of daily living. |
| Provide support and positive reinforcement during activities. | Reassure the patient with continuous supervision until recovery is achieved. |
More Esophageal Varices Nursing Diagnosis
Nursing References
Ackley, B. J., Ladwig, G. B., Makic, M. B., Martinez-Kratz, M. R., & Zanotti, M. (2020). Nursing diagnoses handbook: An evidence-based guide to planning care. St. Louis, MO: Elsevier. Buy on Amazon
Gulanick, M., & Myers, J. L. (2022). Nursing care plans: Diagnoses, interventions, & outcomes. St. Louis, MO: Elsevier. Buy on Amazon
Ignatavicius, D. D., Workman, M. L., Rebar, C. R., & Heimgartner, N. M. (2020). Medical-surgical nursing: Concepts for interprofessional collaborative care. St. Louis, MO: Elsevier. Buy on Amazon
Silvestri, L. A. (2020). Saunders comprehensive review for the NCLEX-RN examination. St. Louis, MO: Elsevier. Buy on Amazon
Disclaimer:
Please follow your facilities guidelines and policies and procedures. The medical information on this site is provided as an information resource only and is not to be used or relied on for any diagnostic or treatment purposes. This information is not intended to be nursing education and should not be used as a substitute for professional diagnosis and treatment.

