Last updated on February 20th, 2023 at 09:19 am
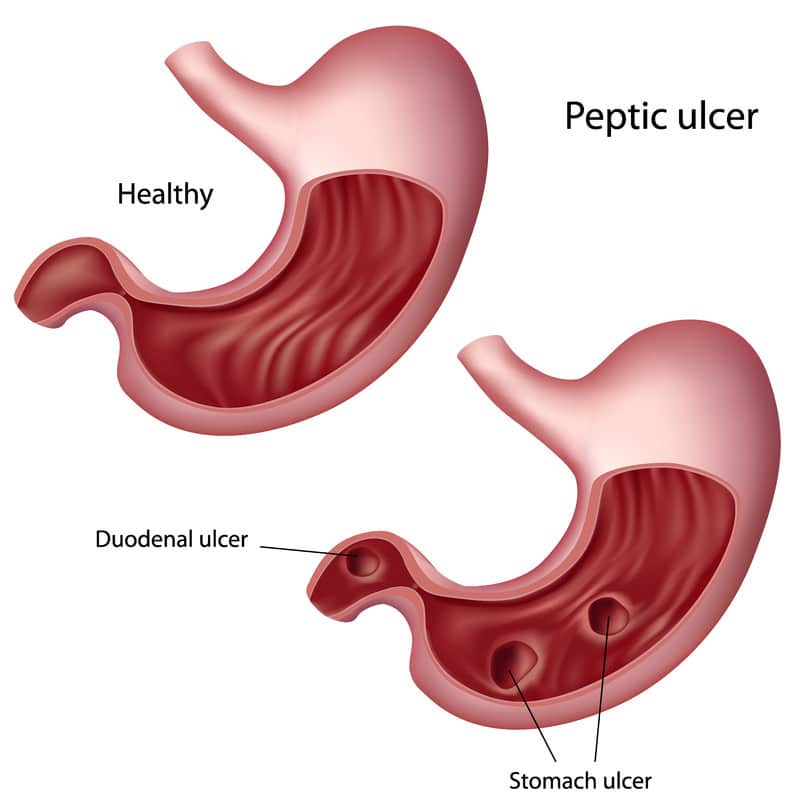
Peptic Ulcer Disease is a medical condition that involves the formation of open sores or ulcers on the stomach’s lining and/or the upper part of the small intestine (duodenum).
Most patients with peptic ulcer disease PUD have stomach pain as the first symptom.
Both gastric and duodenal ulcers can be caused by the infection of the bacteria H.pylori, which is usually considered as a part of the normal flora of the upper digestive tract.
Contrary to common belief, spicy foods do not result to peptic ulcers, but they can aggravate the symptoms and make them even worse.
The same is true with having high stress levels.
Signs and Symptoms of Peptic Ulcer Disease
- Stomach pain that can be described as “burning”
- Bloating or belching
- Feeling of fullness
- Intolerance to fatty foods
- Chest pain or heartburn
- Nausea and/or vomiting.
Long-term or severe symptoms include:
- Vomiting – which may have red or black color (indicating blood)
- Stool color changes – dark blood or black, tarry stools
- Trouble breathing
- Feeling faint
- Loss of appetite
- Unexplained weight loss
Causes and Risk Factors of Peptic Ulcer Disease
The stomach and the rest of the gastro-intestinal tract has a mucous layer that acts as a coating to protect the tissues from the damage that the stomach acid might cause.
However, increased stomach acid and/or the destruction of this coating may result to the development of peptic ulcers.
H. pylori is a bacterium that can normally be found in the upper GI tract in 3 out of 4 people.
It can produce an enzyme called urease that can neutralize the stomach acid, thus weakening the stomach lining.
Close contact such as kissing, as well as food and water are the probable method of transmission of H. pylori. Regular use of pain medications, particularly non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen, can cause irritation and eventual inflammation of the stomach and small intestine’s lining.
Steroids, low-dose aspirin, anticoagulants, and other medications, when taken with NSAIDs, may increase the risk of developing peptic ulcers. Smoking, eating spicy foods, drinking alcohol, and chronic stress may worsen the symptoms of peptic ulcer disease.
Complications of Peptic Ulcer Disease
- Stomach perforation. If left untreated, peptic ulcers can create a hole in the stomach or small intestine’s lining. This can lead to serious infections, such as peritonitis of the abdominal cavity.
- Internal bleeding. This is suspected in severe peptic ulcer disease wherein there is evidence of dark red or black tarry stools, and/or vomiting blood. The blood loss can be slow but progressive, and may put the patient at risk for anemia, which then requires blood transfusion.
- Gastric cancer. People with H. pylori infections such as peptic ulcer disease has a greater risk of developing gastric cancer.
- GI obstruction. Peptic ulcers can cause blockage of the food’s passageway, resulting to symptoms such as weight loss, vomiting, and feeling of fullness.
Diagnosis of Peptic Ulcer Disease
- Physical examination and history taking – to check for food habits and stress levels, as well as physical symptoms of peptic ulcer disease
- H.pylori test – H.pylori can be detected from stool or vomit, but the most accurate one is the breath test. In the breath test, the patient is asked to eat or drink a substance containing radioactive carbon, then he/she will blow into a bag. The presence of carbon dioxide in the breath means that H.pylori broke down the radioactive carbon in the stomach; this indicates a positive H.pylori result. Patients on regular antacids will be asked to stop taking them for a period of time to prevent false negative results.
- Endoscopy – to visualize the digestive tract by means of inserting an endoscope, a thin and flexible tube that comes with a camera and light. Endoscopy can also be used to perform a biopsy, collecting a sample of stomach and/or small intestine tissue.
- Ambulatory acid (pH) probe test – to check for the frequency and duration of acid reflux by means of inserting a thin catheter from the nose down to the esophagus
- Barium swallow, GI X-ray or Upper gastrointestinal series – to visualize the upper gastrointestinal system by means of asking a patient to swallow a barium liquid that will coat the digestive tract, making the peptic ulcers easier to visualize.
Treatment of Peptic Ulcer Disease
- Medications
- Antibiotics against H. pylori. To eradicate H.pylori, the doctor may need to prescribe a combination of antibiotics for about two weeks. These may include amoxicillin, levofloxacin, metronidizole, and clarithromycin.
- Antacids are helpful in neutralizing stomach acid. These include Tums, Rolaids, and Mylanta. Side effects of antacids include kidney disorders and diarrhea.
- H2-receptor blockers. These medications reduce the production of stomach acid. H2-receptor blockers include famotidine, cimetidine, and nizatidine. Compared to the quick relief provided by antacids, H2-receptor blockers take time to act but provides long-term relief, reducing the production of acid for a maximum of 12 hours.
- Proton-pump inhibitors. These medications work by reducing the amount of stomach acid. They include omeprazole and lansoprazole.
2. Lifestyle changes. Smoking cessation and reduced alcohol intake can prevent worsening of ulcer symptoms. Consistent stress management and avoidance of spicy foods should also be included to promote ulcer healing.
Nursing Diagnosis for Peptic Ulcer Disease
Peptic Ulcer Nursing Care Plan 1
Nursing Diagnosis: Imbalanced Nutrition: Less than Body Requirements related to abdominal pain secondary to Peptic Ulcer Disease, as evidenced by burning stomach pain, bloating, weight loss, nausea and vomiting, loss of appetite, heartburn
Desired Outcome: The patient will be able to achieve a weight within his/her normal BMI range, demonstrating healthy eating patterns and choices.
| Nursing Interventions for Peptic Ulcer Disease | Rationale |
| Explore the patient’s daily nutritional intake and food habits (e.g. mealtimes, duration of each meal session, snacking, etc.) | To create a baseline of the patient’s nutritional status and preferences. |
| Create a daily weight chart and a food and fluid chart. Discuss with the patient the short term and long-term nutrition and weight goals related to peptic ulcer disease. | To effectively monitory the patient’s daily nutritional intake and progress in weight goals. |
| Help the patient to select appropriate dietary choices to avoid spicy foods and limit alcohol and coffee intake. | To promote ulcer healing and healthy food habits. Caffeine is a stimulant of gastric acid production. Decaffeinated coffee or tea can still stimulate gastric acid secretion. |
| Refer the patient to the dietitian. | To provide a more specialized care for the patient in terms of nutrition and diet in relation to newly diagnosed peptic ulcer disease. |
| Administer the prescribed medications for peptic ulcer disease. | To reduce stomach acid production or neutralize the stomach acid, relieving the burning stomach pain and helping the patient to have a better appetite. |
Peptic Ulcer Nursing Care Plan 2
Nursing Diagnosis: Acute Pain related to abdominal muscle spasms secondary to peptic ulcer disease as evidenced by pain score of 10 out of 10, verbalization of chest pain or heartburn after eating, guarding sign on the chest or abdomen
Desired Outcome: The patient will demonstrate relief of pain as evidenced by a pain score of 0 out of 10, stable vital signs, and absence of restlessness.
| Nursing Interventions for Peptic Ulcer Disease | Rationale |
| Administer prescribed medications that alleviate the symptoms of heart burn/ stomach pain. | Antibiotics such as amoxicillin can kill H.pyloriAntacids are helpful in neutralizing stomach acid. H2-receptor blockers reduce the production of stomach acid. Proton-pump inhibitors work by reducing the amount of stomach acid. |
| Assess the patient’s vital signs and characteristics of pain at least 30 minutes after administration of medication. | To monitor effectiveness of medical treatment for the relief of heartburn and stomach pain. The time of monitoring of vital signs may depend on the peak time of the drug administered. |
| Teach the patient on how to perform non-pharmacological pain relief methods such as deep breathing, massage, acupressure, biofeedback, distraction, music therapy, and guided imagery. | To reduce stress levels, thereby relieving the symptoms of peptic ulcer disease, especially stomach pain and heartburn. |
| Encourage the patient to follow appropriate mealtimes and meal portions. | To ensure that the patient does not eat a huge meal, or that he/she does not eat late at night/ before bedtime as both of these may trigger nausea/vomiting. |
Peptic Ulcer Nursing Care Plan 3
Nursing Diagnosis: Deficient Knowledge related to repetitive incidents of GI bleeding secondary to peptic ulcer disease as evidenced by the reappearance of symptoms, including black-colored stool, abdominal cramps, bright red-colored vomitus, lightheadedness, weakness, and skin pallor.
Desired Outcomes:
- The client will demonstrate full awareness of peptic ulcer disease, the disease process, treatment management, and possible outcome.
- The client will establish a consistently positive response to the treatment plan.
- The client will verbalize full commitment to the continuance of lifestyle change and improvement.
| Nursing Interventions for Peptic Ulcer Disease | Rationale |
| Evaluate the client’s awareness about the peptic ulcer disease or if they have any mistaken info about it. Also, check the patient’s level of understanding or misconception about lifestyle habits and medical care management. | There is some inaccurate information spreading nowadays, one common example is how lifestyle habits play a part in causing peptic ulcer disease. Therefore, factual and authentic details must be provided to the patient. Educating the client about the Vital information is a must. These include the benefits of the client’s compliance in taking prescribed medications, changes in daily habits that contribute to developing GI bleeding, thus leading to Peptic ulcer disease. Just be sure to make the explanation easier to be understood, using common terms and avoiding complex terminologies. Spend enough time to answer clients’ questions and ensure them that whenever they have queries or concerns. Be not hesitant to ask. |
| Expound the pathophysiology of disease in detail and emphasize how it affects the body processes, but avoid using medical jargon as much as possible. | Having an in-depth understanding of the disease process promotes adherence and compliance to the patients to the recommended treatment plan and lifestyle modification. These will benefit the patient not only in treating the disease itself, but also to avoid recurrence of symptoms and prevent associated complications. |
| Educate the patient about what signs and symptoms should be watched for and advise them to report them immediately with their healthcare provider. | Being well informed of the signs and symptoms is an advantage in establishing a prompt response to the treatment. |
| Have a thorough explanation of all possible therapeutic options, their principles, and how the patient can benefit from them. | The proper use of antibiotics and other medications like acid suppressants promotes the fast recovery of an ulcer. Medicine should be taken as prescribed by the healthcare provider. Non-pharmacological technique to relieve pain includes deep breathing, massage, relaxation, and reduction of stress level |
| Discuss the significance of lifestyle modification as preventive measures against additional complications or recurrence of peptic ulcer disease. Changes in lifestyle habits such as alcohol abuse, too much coffee intake and another high in caffeine drink, improper intake, and prolonged use of medications like aspirin or other nonsteroidal anti-inflammatory drugs are important to reduce the risk of developing exacerbationDiscuss the client’s dietary requirements. | Alongside treatment plans and lifestyle changes, a well-balanced diet is also essential to promote healing and healthy well-being. Ideally, this planning is done with a nutritionist and/or a dietitian. A diet plan is usually initiated to supply the necessary nutrition requirements. |
Peptic Ulcer Nursing Care Plan 4
Anxiety
Nursing Diagnosis: Anxiety related to the nature of the disease secondary to peptic ulcer disease as evidenced by verbal reports of fear and worry.
Desired Outcomes:
- The patient will start discussing their feelings, concerns, and worries.
- The patient will be able to report which stressors most likely affect them, and explore what daily habits can help them to overcome those stressors.
- The client will exhibit coping patterns effectively with the modality of available treatment, pharmacologic and non-pharmacologic methods.
- The client will verbalize feelings of comfort, confidence, and safety. As a result, the patient’s anxiety level will be reduced and the risk for anxiety attacks will be lowered.
| Nursing Interventions for Peptic Ulcer Disease | Rationale |
| Evaluate the client’s psychological and physiological status and level of anxiety. | People suffering from Peptic ulcer disease experience anxiousness, though the level of their anxiety is not usually manifested. Encourage the client to open up their thoughts and ensure to them that we welcome them if they do have any questions. Be patient in explaining to them the important details because they tend to be sensitive because of fear. |
| Recognize the understanding of the client’s anxiety. | Recognize the client’s feelings, be attentive in listening to what they share. It develops the feeling of trust and acceptance between the client and healthcare provider. This may help the client to acknowledge anxiety and fear. |
| Give support by allowing the client to verbalize their fears and concerns freely. | Sustain a trustful relationship with the client as they express themselves gives assurance that they can speak up openly. It gives comfort and relieves uneasiness that helps in reducing anxiety and stress levels.. |
| Communicate using simple language, easily understood statements when giving direction to the client. | Clients experiencing moderate to severe anxiety may not be able to understand statements that are complex, vague, and even lengthy instructions. The right choice of words is also necessary so we can catch their interest and also avoid their thoughts being triggered. |
| Maintain a calm and quiet environment to minimize stressors and stimuli. | External stimuli may escalate anxiety to panic attacks such as a noisy environment. Avoid noise, too loud conversation, and equipment around the client. In dealing with clients, establishing a non-threatening environment develops security and peace for them. It will help to put the client at ease. |
| Ensure emotional support to the client. | Extending emotional support to the client will provide a calm and relaxing feeling that may brighten up their mood and ease their stress and anxiety. Strong emotional support offers unconditional comfort measures. Promote wellness, keep them reminded with the positive coping strategies, and refrain from triggers. |
| Help the patient in developing techniques that reduce anxiety levels and stress management strategies. These measures include biofeedback, positive imagery, and behavior modification. | Aside from pharmacological treatments, there are also nonchemical ways that are effective in dealing with anxiety. Learning and with a regular habit of practicing these techniques provide confidence to the client in overcoming anxiety. . |
Peptic Ulcer Nursing Care Plan 5
Risk for deficient fluid volume
Nursing Diagnosis: Risk for Deficient Fluid Volume related to gastrointestinal (GI) bleeding secondary to peptic ulcer disease.
Desired Outcomes:
- The client will be normovolemic as indicated by a systolic blood pressure greater or equal to 90 mm Hg (or client’s baseline), absence of orthostasis, normal skin turgor.
- The patient will demonstrate a maintained fluid volume as shown by normal hematocrit and hemoglobin count.
- The client will verbalize the absence of abdominal cramps and lightheadedness and only a few incidents of black-colored stool and vomiting.
- The patient will report reduced fatigability, increased comfort, and energy levels.
| Nursing Interventions for Peptic Ulcer Disease | Rationale |
| Observe the patient for the signs of hematemesis or melena. | Hematemesis is described as vomiting of blood, it can be bright red or coffee-ground emesis. Dark brown colored vomitus with granular material that looks like coffee ground. Melena refers to a black tarry stool. In Peptic ulcer disease, both hematemesis and melena are caused by bleeding sores or ulcers that are developed in the small intestine. It is important to look out for the quantity, color, consistency, and frequency of blood passage. These are important details that help in locating the origin and location of the bleeding site. In cases of hematemesis, specific questions are asked to differentiate it from hemoptysis, as sometimes patients get confused with these two. |
| Monitor the patient’s client’s vital signs, specifically blood pressure and heart rate. Take note of any signs of orthostasis. . | Gastrointestinal bleeding happens when the ulcer through the gastric mucosal layer erodes. As bleeding continues to occur, the client may have severe loss of body fluids. Changes in vital signs like decrease in Blood pressure and increase in heart rate in sitting or standing position are among the early and common manifestations of excessive fluid loss and decrease in blood volume. Physical symptoms may also develop briskly if blood volume continues to drop. |
| Record the client’s daily fluid intake and output. Output level includes the amount of urine, gastric secretion, and other losses such as vomitus. | As gastrointestinal bleeding continues, there is a decrease in the blood volume in our body. The kidney’s compensatory mechanism is to reabsorb water into circulation to support blood circulation and This may result in decreased urine output. A reduction in circulatory blood volume will result in a decrease in renal perfusion and decreased urine output. The considered normal urine output is not less than 30ml/ hour. An accurate record of measurement of fluid intake and output is necessary to identify the fluid status of the patient. Notify your healthcare provider immediately if urine output is less than 30ml per hour for two consecutive hours. |
| Obtain samples for laboratory studies as requested. | If gastric bleeding occurs, the levels of hemoglobin and hematocrit may be affected. Blood tests play a significant role in assessing the bleeding status. It will also manifest if excessive blood loss is happening. Blood levels will be monitored regularly in a period to avoid Anemia and other complications. |
| Check the patency of the intravenous line and administer intravenous fluids, volume expanders, and blood products as ordered. | Hypovolemic or hemorrhagic shock may happen if there is severe blood loss. Fluids are important to maintain hydration. Intravenous access is obtained immediately to start parenteral fluids to prevent or treat shock. Patients are closely monitored. For severe bleeding, massive blood loss happens and transfusion may be required until the intravascular volume is restored and ongoing blood loss has been replaced. |
More Peptic Ulcer Disease Nursing Diagnosis
- Impaired comfort related to abdominal pain and discomfort associated with peptic ulcer disease.
- Impaired skin integrity related to prolonged use of nonsteroidal anti-inflammatory drugs (NSAIDs).
- Risk for bleeding related to ulceration and erosion of blood vessels in the stomach or duodenum.
- Impaired gas exchange related to bleeding from a peptic ulcer.
- Impaired bowel elimination related to nausea, vomiting and diarrhea associated with peptic ulcer disease.
- Impaired oral mucous membrane related to nausea and vomiting
Impaired physical mobility related to abdominal pain and discomfort. - Risk for infection related to the presence of an ulcer in the stomach or duodenum.
Nursing References
Ackley, B. J., Ladwig, G. B., Makic, M. B., Martinez-Kratz, M. R., & Zanotti, M. (2020). Nursing diagnoses handbook: An evidence-based guide to planning care. St. Louis, MO: Elsevier. Buy on Amazon
Gulanick, M., & Myers, J. L. (2022). Nursing care plans: Diagnoses, interventions, & outcomes. St. Louis, MO: Elsevier. Buy on Amazon
Ignatavicius, D. D., Workman, M. L., Rebar, C. R., & Heimgartner, N. M. (2020). Medical-surgical nursing: Concepts for interprofessional collaborative care. St. Louis, MO: Elsevier. Buy on Amazon
Silvestri, L. A. (2020). Saunders comprehensive review for the NCLEX-RN examination. St. Louis, MO: Elsevier. Buy on Amazon
Disclaimer:
Please follow your facilities guidelines and policies and procedures. The medical information on this site is provided as an information resource only and is not to be used or relied on for any diagnostic or treatment purposes. This information is not intended to be nursing education and should not be used as a substitute for professional diagnosis and treatment.

