Asthma is a chronic condition that involves the narrowing and/or swelling of the airways, causing difficulty of breathing and triggering of cough.
This may also include excessive production of mucus. Asthma is sometimes referred to as reactive airway disease or bronchial asthma.
There is no cure for asthma, but the symptoms can be managed and controlled effectively. Asthma can interfere with a patient’s activities of daily living and also put him/her at risk for asthma attacks.
If you would like the full-size PDF sent, please see below.
Signs and Symptoms of Asthma
- Shortness of breath
- Chest tightness or pain
- Wheezing upon exhalation, especially in children
- Coughing
- Phlegm at times (most asthma cases are non-productive)
- Sleeping problems due to coughing or breathlessness
- Tiredness
- Feelings of anxiety or panic
- Rapid breathing
Causes of Asthma
The exact cause of asthma is unknown. Experts believe that asthma is caused by genetic and environmental factors.
Asthma attacks or flare-ups may be triggered by different environmental factors. Exercise-induced asthma may occur if the patient’s exercise and physical activity results to an asthma attack. This becomes worse if the patient is exercising in a cold environment where the air is dry.
Allergy-induced asthma happens when airborne substances such as mold spores, pollen, insect waste, pet dander, or skin particles trigger the asthma. Occupational asthma occurs in the workplace where gases, dust, chemical fumes or other workplace irritants may be present.
Other triggers of asthma include respiratory infections, air pollutants such as cigarette smoke, vehicular smoke, emotional stress, some medications such as aspirin and non-steroidal anti-inflammatory drugs (NSAIDS) like ibuprofen and naproxen, some sulfites and preservatives. Gastroesophageal reflux disease (GERD) may also give rise to asthma symptoms.
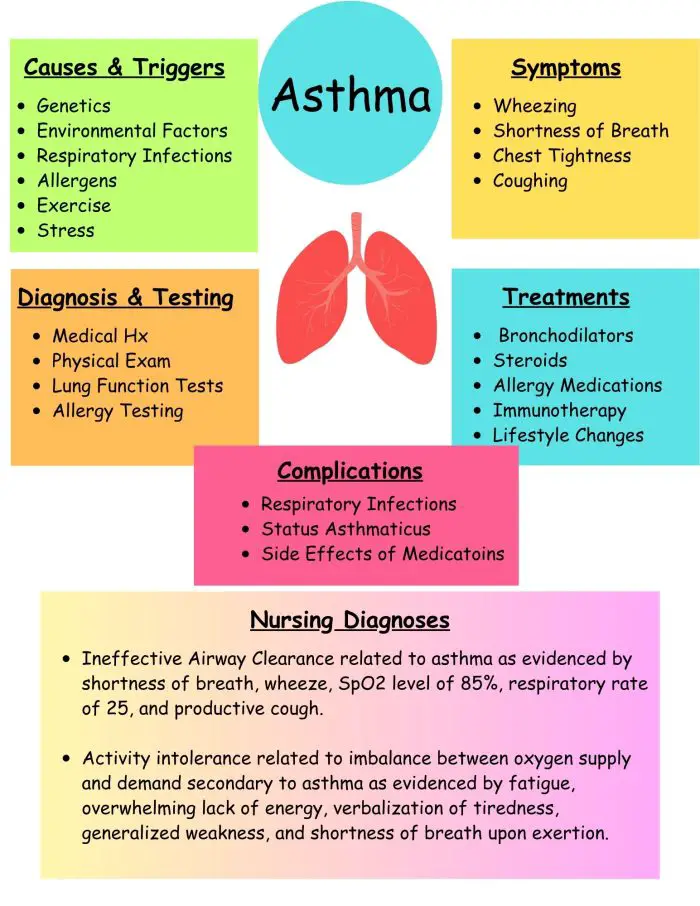
Diagnosis of Asthma
- Physical examination – auscultation of wheeze, inspection of ear, nose, throat and airways, looking for any chest retractions or signs of cyanosis, checking for respiratory rate and oxygen saturation levels
- Lung function tests – spirometry and peak flow meter; done before and after taking a bronchodilator
- Imaging – chest X-ray
- Allergy testing
- Sputum test – to check if there are any eosinophils in the sputum
Treatment for Asthma
Oxygen
- Long-term asthma medications. These are used on a daily basis to control the asthma symptoms and prevent an asthma attack. These include:
- Inhaled corticosteroids such as budesonide, fluticasone, and beclomethasone
- Leukotriene modifiers, such as oral montelukast and zileuton
- Combination inhalers – combined corticosteroid and long-acting beta agonist, such as fluticasone-salmeterol (e.g. Advair HFA), budesonide-formoterol (Symbicort), formoterol-mometasone (Dulera) and fluticasone furoate-vilanterol (Breo Ellipta).
- Theophylline – relaxes the airway muscles, allowing the airways to remain open; requires blood tests to determine toxicity levels
- Quick-relief or rescue medications. These medications are used during asthma attacks for short-term relief. They may be used before exercise.
- Short-acting beta agonists – bronchodilators such as albuterol and levalbuterol.
- Anticholinergic agents – also used in chronic bronchitis and emphysema. These include ipratropium (Atrovent) and tiotropium (Spiriva)
- Oral and intravenous corticosteroids – alleviate airway inflammation. These include prednisone and methylprednisolone.
- Allergy medications for allergy-induced asthma
- Biologics for severe asthma include omalizumab (Xolair) and mepolizumab (Nucala)
- Bronchial thermoplasty. This procedure includes heating up the lung airways using an electrode. This is done over 3 clinic visits.
Nursing Care Plans for Asthma
Ineffective Airway Clearance
Nursing Diagnosis: Ineffective Airway Clearance related to asthma as evidenced by shortness of breath, wheeze, SpO2 level of 85%, respiratory rate of 25, and productive cough
Desired Outcome: The patient will be able to maintain airway patency and improved airway clearance as evidenced by being able to expectorate phlegm effectively, respiratory rates between 12 to 20 breaths per minutes, oxygen saturation within the target range, and verbalize ease of breathing.
Nursing Interventions for Ineffective Airway Clearance
Assess the patient’s vital signs and characteristics of respirations at least every 4 hours. Assess breath sounds via auscultation. To assist in creating an accurate diagnosis and monitor effectiveness of medical treatment. Wheeze is one of the important signs of asthma.
Encourage coughing. Suction secretions as needed. To help clear thick phlegm that the patient is unable to expectorate.
Administer supplemental oxygen, as prescribed. Discontinue if SpO2 level is above the target range, or as ordered by the physician. To increase the oxygen level and achieve an SpO2 value within the target range.
Administer the prescribed asthma medications (e.g. bronchodilators, steroids, or combination inhalers / nebulizers). Bronchodilators: To dilate or relax the muscles on the airways. Steroids: To reduce the inflammation in the lungs.
Elevate the head of the bed and assist the patient to assume semi-Fowler’s position. Head elevation and proper positioning help improve the expansion of the lungs, enabling the patient to breathe more effectively.
Activity Intolerance
Nursing Diagnosis: Activity intolerance related to imbalance between oxygen supply and demand secondary to asthma as evidenced by fatigue, overwhelming lack of energy, verbalization of tiredness, generalized weakness, and shortness of breath upon exertion
Desired Outcome: The patient will be able to demonstrate active participation in necessary and desired activities and demonstrate an increase in activity levels.
Nursing Interventions for Activity Intolerance
Assess the patient’s activities of daily living, as well as actual and perceived limitations to physical activity. Ask for any form of exercise that he/she used to do or wants to try. To create a baseline of activity levels and mental status related to fatigue and activity intolerance.
Encourage progressive activity through self-care and exercise as tolerated. Explain the need to reduce sedentary activities such as watching television and using social media in long periods. Alternate periods of physical activity with 60-90 minutes of undisturbed rest. To gradually increase the patient’s tolerance to physical activity. To prevent asthma attack by allowing the patient to pace activity and to have rest periods.
Teach deep breathing exercises and relaxation techniques. Provide adequate ventilation in the room. To allow the patient to relax while at rest and to facilitate effective stress management. To allow enough oxygenation in the room.
Refer the patient to physiotherapy / occupational therapy team as required. To provide a more specialized care for the patient in terms of helping him/her build confidence in increasing daily physical activity.
Ineffective Breathing Pattern
Nursing Diagnosis: Ineffective Breathing Pattern related to inadequate pulmonary ventilation, secondary to asthma, as evidenced by shortness of breath, coughing, cyanosis, nasal flaring, changes in the depth of breathing, excessive use of accessory muscles, presence of respiratory noise, and tachypnea.
Desired Outcomes:
- The patient’s abnormal breathing pattern will be corrected, as evidenced by a normal respiratory pattern, with no evidence of dyspnea noted.
- The nurse will note that the use of diaphragmatic compression is evident, ABG values are within the prescribed ranges, and there is evidence of comfortable breathing, either vocally or by the patient’s conduct.
Nursing Interventions for Ineffective Breathing Pattern
Monitor the patient and take any necessary vital signs readings while he/she is in a state of distress. During the first stage of hypoxia and hypercapnia, the BP, RR, and HR likely elevate. And when the patient’s condition deteriorates to the point where blood pressure and heart rate fall, respiratory failure might occur.
Evaluate the rate, depth, and rhythm of the patient’s breathing. When the patient’s usual breathing pattern or rhythm changes, there is a strong probability that an impending ailment or disease state is developing; in particular, this may be an early warning sign of oncoming respiratory distress.
Determine the degree to which the patient is experiencing anxiety. There may be a sense of panic when the patient is experiencing difficulty breathing adequately. Hence, assessing his/her level of anxiety would be beneficial in mitigating its course or progression.
Listen to the patient’s breathing and note any abnormalities, including any wheezes or stridor. If unusual sounds persist, it could indicate a worsening condition or the emergence of new complications. It should be noted that patients with chronic respiratory issues like asthma may be more susceptible to lung infections (e.g., pneumonia).
Observe any signs and indicators of shortness of breath (dyspnea) that may present as retractions of the chest, excessive use of accessory muscle, and nasal flaring. This is an essential indicator that the patient may be suffering from breathing issues as these are signs of possible respiratory distress. When there is significant inspiratory effort, the breathing pattern is noticeably altered due to difficulty pumping air into and out of the lungs.
Regularly monitor the patient’s oxygen saturation. Oxygen saturation refers to the percentage of blood hemoglobin that is saturated by oxygen. 95-100 percent oxygen saturation is considered normal, and deviations within this baseline level indicate inadequate ventilation. It may arise from several causes, but it is often correlated with asthma if blockages are present (e.g., mucus) in the airway passage.
Regularly monitor the patient’s arterial blood gas (ABG). Individuals who suffer from mild to moderate persistent asthma may be at risk of developing respiratory alkalosis. It is expected that the respiratory rate and depth will rise in the presence of hypoxemia. On the other hand, respiratory acidosis is a concerning finding since it often suggests that respiratory failure is on the way and that mechanical ventilation may be required in the near future.
Require the patient to have a dedicated rest schedule incorporated into his/her daily routine. A common side effect of having an improper breathing pattern is exhaustion due to the additional work required to breathe normally. Metabolic rate and oxygen consumption rise with exercise, and for that reason, periodic rest between care activities should be incorporated.
Suggest to the patient to inhale and exhale via pursed lips. When the patient breathes with his/her lips pursed, he/she is allowing more fresh air to enter the lungs while expelling old air they’ve been holding in.
Encourage calm, deep breathing while staying close to the client. The nurse should inform the patient and any other important individuals that they are closely watching their situation and will intervene if necessary. Having a trusted and reliable person in the room can make the patient feel more secure; hence, reinforcing a support system.
Anxiety
Nursing Diagnosis: Anxiety related to uncontrollable status shifts, secondary to asthma as evidenced by shortness of breath, restlessness, uneasiness, tachycardia, continuous requested presence in the room, and tachypnea.
Desired Outcome: The patient will demonstrate effective coping as evidenced by a reported decrease in the degree of anxiety and reduced anxiousness in the form of a calmer demeanor and more cooperative conduct.
Nursing Interventions for Anxiety
Observe the patient for symptoms of nervousness or anxiety such as:
● Visible signs of panic attacks
● Trepidation or fearfulness
● Restlessness
● Uneasiness
● Tachycardia
● Hands or feet that are either cold or sweaty
● Dyspnea Asthma may also be exacerbated by anxiety. And when this happens, the patient tends to exhibit a fast, shallow breathing pattern.
Monitor the level of oxygen in the patient’s blood. Oxygen saturation refers to the percentage of blood hemoglobin saturated by oxygen. 95-100 percent oxygen saturation is considered normal. Establishing the oxygen saturation level would provide baseline data on the patient’s risk of developing hypoxia which is often noted in asthma attacks.
Ensure the patient is at ease and comfortable by providing amenities like a quiet, peaceful space and soothing music. Remaining calm and exerting less inspiratory effort makes breathing easier and conserves the patient’s energy equally.
Assist the patient in understanding each step of the process by thoroughly explaining the procedure clearly and concisely. When the treatment plan is more understood, the patient’s anxiety may lessen. Consequently, the patient’s breathing pace is unlikely to change since he/she will be less apprehensive and concerned.
Maintain constant communication with the patient’s family and loved ones to keep them informed of the patient’s improvement. Anxiety can readily be passed on from family members or significant others to the patient. A peaceful and stress-free environment is of utmost importance, especially when the patient is easily perturbed and troubled. Most likely, it would also ease certain risks of complications developing. Hence, disclosing information to family members would help alleviate their fears and anxiety. Making this step contributes to the promotion of a relaxing, stress-free atmosphere.
Assure the patient and anyone involved that he/she will be closely monitored and that immediate intervention will be made. Having a trusted and reliable person in the room can make the patient feel more secure and at ease.
Observe the patient and support him/her by suggesting to take a slow, deep breath. To enhance the patient’s health prior to any complications arising and to help him/her progressively calm down.
Suggest relaxation techniques for the patient to employ, such as gradual decrease of muscle tension using progressive muscle techniques, diaphragmatic breathing, pursed-lip breathing, guided imagery, and positive affirmations (e.g., relax, take a deep breath, and let go). Asthma attacks can be triggered by panic episodes brought on by anxiety. Hence, techniques like deep breathing and meditation can help alleviate stress and anxiety.
Health-Seeking Behaviors: Prevention of Asthma Attack
Nursing Diagnosis: Health-Seeking Behaviors: Prevention of Asthma Attack related to an expressed desire to avoid and correct situations impetus of asthmatic episodes, as evidenced by an increased interest for better control over health practices, the impact of environmental factors and behavioral factors on health, and an increase in the number of attacks
Desired Outcomes:
- The parents and the patient will communicate their comprehension of the triggering agents that may induce an asthma attack.
- Avoidance strategies will also be communicated effectively.
Nursing Interventions for Health Seeking Behaviors
Examine the patient’s medical history for information such as the incidence of respiratory illnesses, triggering determinants, and the kind of therapies or actions taken to improve the patient’s health. Respiratory changes or infections can trigger asthma attacks, and determining its incidence can provide baseline information to keep the patient healthy.
Identify allergies in the patient’s family and what causes an attack, and the behaviors that ensue after the attack. Indicates whether there is a history of reactive airway diseases, eczema, allergic rhinitis, or urticaria within the family. In addition, it is not uncommon to link reactive airway illnesses to asthma, as it is used to describe suspected cases of asthma that have yet to be diagnosed.
Determine if the patient is taking any over-the-counter medications, and if so, what kind they are and what effects they are having. Respiratory infections are often treated with over-the-counter drugs, and acquiring this information would help determine the kind of OTC medications that may interfere with prescribed medications and cause a worsening of the respiratory conditions or attacks.
Inform the patient to maintain a safe distance or keep away from people with respiratory infections. Respiratory infections are infectious, and they could potentiate and trigger asthma attacks. Inhaling aerosolized droplets could be avoided by taking preventative actions such as staying away from those who are unwell.
Encourage the patient to use tissues to cover the mouth while coughing or sneezing and properly dispose of tissues when he/she is done using them. To prevent the spread of bacteria by inhalation of aerosolized droplets.
As a precaution, suggest to parents that they make changes to the patient’s home environment, such as changing filters to reduce exposure to dust and getting rid of common food allergens like peanuts and eggs. To reduce the chance of an attack being triggered.
Explain the disease, its symptoms, as well as probable underlying causes that might trigger an attack. Contains information that can be used to enhance the effectiveness of preventive measures. Adherence to prescribed treatment programs would be improved as patients would find it easier to include something they are familiar with.
Take the time to instruct the patient and parents on correct handwashing procedures and offer time for a follow-up demonstration. Avoids the transmission of pathogens from close contacts, such as touching.
Contact local groups that can support and educate the patient. These organizations provide assistance to families with an asthmatic child or family member.
Other Nursing Diagnosis
Nursing References
Ackley, B. J., Ladwig, G. B., Makic, M. B., Martinez-Kratz, M. R., & Zanotti, M. (2020). Nursing diagnoses handbook: An evidence-based guide to planning care. St. Louis, MO: Elsevier.
Alizadeh, A., Dyck, S. M., & Karimi-Abdolrezaee, S. (2019). Traumatic Spinal Cord Injury: An Overview of Pathophysiology, Models and Acute Injury Mechanisms. Frontiers in neurology, 10, 282. https://doi.org/10.3389/fneur.2019.00282
Gulanick, M., & Myers, J. L. (2017). Nursing care plans: Diagnoses, interventions, & outcomes. St. Louis, MO: Elsevier.
Hills, Teresa E. MSN, RN, ACNP-BC, CNRN. Caring for patients with a traumatic spinal cord injury. Nursing 50(12):p 30-40, December 2020. | DOI: 10.1097/01.NURSE.0000721724.96678.5a
Ignatavicius, D. D., Workman, M. L., Rebar, C. R., & Heimgartner, N. M. (2018). Medical-surgical nursing: Concepts for interprofessional collaborative care. St. Louis, MO: Elsevier.
Silvestri, L. A. (2020). Saunders comprehensive review for the NCLEX-RN examination. St. Louis, MO: Elsevier.
Best Nursing Books and Resources
These are the nursing books and resources that we recommend.
NurseStudy.net is a participant in the Amazon Services LLC Associates Program. Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. Please see our Privacy Policy
The Nursing Diagnosis Handbook E-Book: An Evidence-Based Guide to Planning Care
This is an excellent reference for nurses and nursing students. While it is a great resource for writing nursing care plans and nursing diagnoses, it also helps guide the nurse to match the nursing diagnosis to the patient assessment and diagnosis.
This handbook has been updated with NANDA-I approved Nursing Diagnoses that incorporates NOC and NIC taxonomies and evidenced based nursing interventions and much more.
NANDA International Nursing Diagnoses: Definitions & Classification, 2021-2023
All introductory chapters in this updated version of a ground-breaking text have been completely rewritten to give nurses the knowledge they require to appreciate assessment, its relationship to diagnosis and clinical reasoning, and the goal and use of taxonomic organization at the bedside.
Nursing Care Plans: Nursing Diagnosis and Intervention
It contains more than 200 care plans that adhere to the newest evidence-based recommendations.
Additionally, it distinguishes between nursing and collaborative approaches and highlights QSEN competencies.
Disclaimer:
Please follow your facility’s guidelines, policies, and procedures.
The medical information on this site is provided as an information resource only and should not be used or relied on for diagnostic or treatment purposes.
This information is intended to be nursing education and should not be used as a substitute for professional diagnosis and treatment.