Last updated on April 15th, 2023 at 09:52 am
Hypertension, commonly known as high blood pressure, is a chronic medical condition that affects millions of people worldwide. It is a major risk factor for heart disease, stroke, and kidney failure. Nursing diagnosis is an essential component of hypertension management, as it helps nurses to identify the patient’s health problems and develop an effective care plan.
The five hypertension nursing diagnoses discussed in this article are: ineffective health maintenance, ineffective therapeutic regimen management, risk for decreased cardiac output, risk for injury, and anxiety.
For each diagnosis, we will discuss the nursing interventions that can help manage the patient’s condition, as well as the rationale behind these interventions. By understanding these nursing diagnoses and interventions, nurses can provide high-quality care to patients with hypertension and help them achieve better health outcomes.
This article is intended for nurses and other healthcare professionals who work with patients with hypertension. It aims to provide a comprehensive overview of the nursing diagnoses and interventions that are essential for effective hypertension management.
By following the nursing interventions outlined in this article, nurses can help patients manage their blood pressure, reduce their risk of complications, and improve their overall quality of life.
What is Hypertension?
Hypertension, also known as high blood pressure, is a chronic medical condition characterized by elevated blood pressure in the arteries. Blood pressure is the force of blood pushing against the walls of the arteries as the heart pumps blood. When the blood pressure is consistently high, it can lead to serious health problems such as heart disease, stroke, and kidney failure.
Hypertension is a common condition that affects millions of people worldwide. It is often referred to as a “silent killer” because it often has no symptoms, and many people are unaware that they have it until they experience a serious health problem.
The causes of hypertension are not always clear, but several factors can contribute to it, including genetics, lifestyle choices, and underlying medical conditions. Risk factors for hypertension include obesity, smoking, stress, lack of physical activity, and a diet high in salt and saturated fats.
Hypertension can be managed through lifestyle changes, medication, and regular monitoring of blood pressure. It is important for individuals with hypertension to work closely with their healthcare provider to develop a treatment plan that is tailored to their specific needs and health goals.
Causes of Hypertension
Hypertension, or high blood pressure, is a common condition that affects millions of people worldwide. It occurs when the force of blood against the walls of the arteries is consistently too high. While there are many factors that can contribute to the development of hypertension, some of the most common causes include:
- Genetics
- Dietary factors, such as consuming too much sodium or not enough potassium
- Lack of physical activity
- Obesity or being overweight
- Smoking and tobacco use
- Stress and anxiety
Other risk factors for hypertension include age, gender, and family history. Certain medical conditions, such as diabetes and kidney disease, can also increase a person’s risk of developing hypertension.
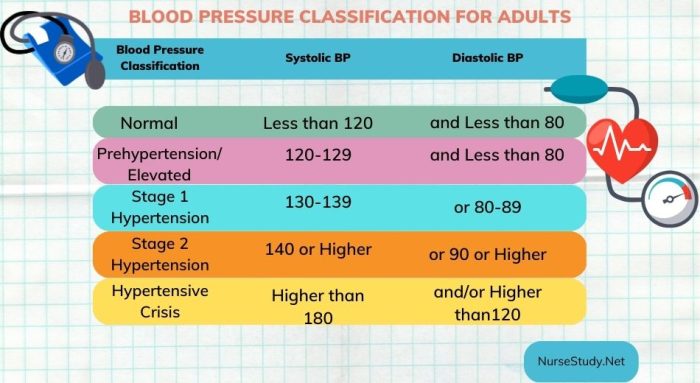
It’s important to note that hypertension often develops gradually over time, and many people may not experience any symptoms until the condition has reached a more advanced stage. Regular blood pressure screenings are essential for early detection and treatment of hypertension.
Signs and Symptoms of Hypertension
Hypertension, also known as high blood pressure, is a silent killer that does not show any visible symptoms in the early stages. However, as the condition progresses, some common signs and symptoms may start to appear. Here are some of the common signs and symptoms of hypertension:
- Headaches: Persistent headaches, especially at the back of the head, can be a sign of hypertension.
- Dizziness: Feeling lightheaded or dizzy can be a symptom of hypertension.
- Shortness of breath: Difficulty breathing or shortness of breath can be a sign of hypertension.
- Chest pain: Chest pain, especially during physical activity, can be a symptom of hypertension.
- Visual changes: Blurred vision or other visual changes can be a sign of hypertension.
- Blood in urine: Blood in the urine can be a symptom of hypertension-related kidney damage.
- Nosebleeds: Although rare, frequent nosebleeds can be a sign of hypertension.
It is important to note that these symptoms are not specific to hypertension and can be caused by other conditions as well. Therefore, it is important to get regular blood pressure checkups to detect hypertension early and prevent complications.
Treatment for Hypertension
Hypertension is a chronic condition that requires lifelong management. The goal of treatment is to reduce blood pressure and prevent complications. Treatment options include lifestyle modifications, medications, and in some cases, surgery. The treatment plan is individualized and based on the patient’s blood pressure level, overall health, and other factors.
Lifestyle modifications that can help lower blood pressure include:
- Reducing salt intake
- Eating a healthy diet rich in fruits, vegetables, and whole grains
- Engaging in regular physical activity
- Maintaining a healthy weight
- Avoiding tobacco and limiting alcohol consumption
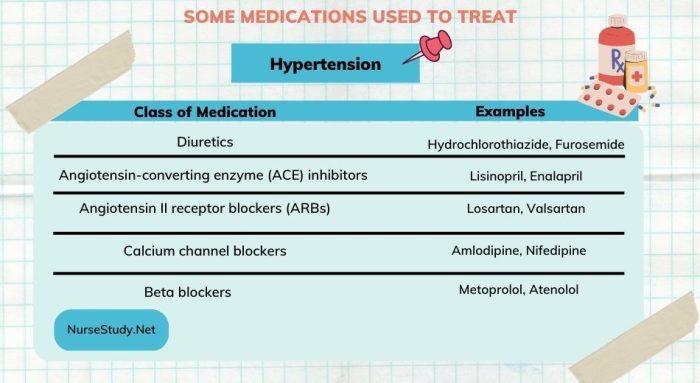
If lifestyle modifications alone are not enough to control blood pressure, medications may be prescribed. There are several classes of medications used to treat hypertension, including: Diuretics, Angiotensin-converting enzyme (ACE) inhibitors, Angiotensin II receptor blockers (ARBs), Calcium channel blockers, and Beta blockers.
In some cases, surgery may be recommended to treat hypertension. This may include renal artery stenosis or pheochromocytoma. However, surgery is typically reserved for cases in which other treatment options have failed.
It is important for patients with hypertension to work closely with their healthcare providers to develop an individualized treatment plan. Regular monitoring and follow-up appointments are essential to ensure that blood pressure is well-controlled and to adjust treatment as needed.
Nursing Process for Hypertension
The nursing process is a systematic approach to patient care that involves assessment, diagnosis, planning, implementation, and evaluation. It is an essential tool for nurses in managing patients with hypertension, as it allows for a comprehensive understanding of the patient’s condition and the development of individualized care plans.
The first step in the nursing process is assessment, which involves gathering information about the patient’s medical history, lifestyle, and current symptoms. This information is used to identify potential risk factors for hypertension and to establish a baseline for monitoring the patient’s condition.
The next step is diagnosis, which involves identifying nursing diagnoses related to the patient’s hypertension. Common nursing diagnoses for hypertension include ineffective health maintenance, risk for decreased cardiac output, and risk for injury related to complications of hypertension.
Once nursing diagnoses have been established, the nurse can begin to develop a plan of care. This plan should be individualized to the patient’s specific needs and should include nursing interventions aimed at addressing the identified nursing diagnoses. Nursing interventions for hypertension may include lifestyle modifications, medication management, and patient education.
Implementation involves carrying out the nursing interventions identified in the plan of care. This may involve administering medications, providing patient education, and monitoring the patient’s vital signs and symptoms. It is important for nurses to document all interventions and patient responses to treatment.
The final step in the nursing process is evaluation, which involves assessing the effectiveness of the nursing interventions and determining if the patient’s condition has improved. If the patient’s condition has not improved, the nurse may need to reassess the plan of care and adjust interventions as necessary.
Overall, the nursing process is an essential tool for nurses in managing patients with hypertension. By using a systematic approach to patient care, nurses can develop individualized care plans that address the unique needs of each patient and improve outcomes.
Hypertension Nursing Diagnosis
Hypertension, also known as high blood pressure, is a common condition that affects millions of people worldwide. It is a chronic medical condition that requires ongoing care and management. As a nurse, it is important to identify nursing diagnoses for patients with hypertension to provide appropriate care and interventions. Here are five common nursing diagnoses for hypertension, along with nursing interventions and rationales.
Ineffective Health Maintenance
Patients with hypertension may have difficulty maintaining a healthy lifestyle, such as following a low-sodium diet, engaging in regular physical activity, and taking medications as prescribed. Ineffective health maintenance is a nursing diagnosis that relates to the patient’s inability to manage their health effectively. Nursing Interventions:
- Educate the patient on the importance of following a low-sodium diet and provide resources for healthy meal planning.
- Encourage the patient to engage in regular physical activity, such as walking or swimming, and provide resources for exercise programs.
- Assist the patient with medication management, including reminders to take medications and instructions on how to properly administer them.
Rationale: These interventions aim to promote healthy behaviors and encourage the patient to take an active role in managing their health.
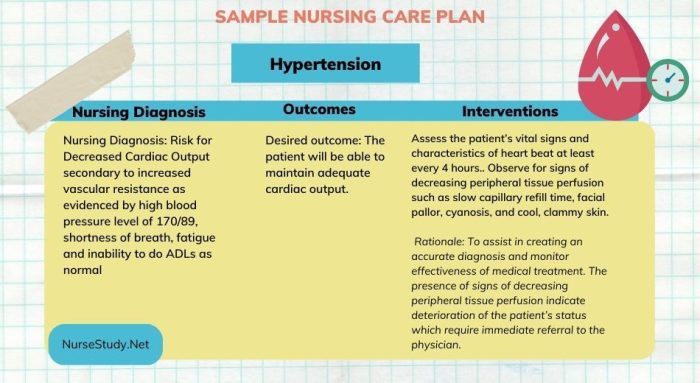
Risk for Decreased Cardiac Output
Hypertension can lead to decreased cardiac output, which refers to the amount of blood pumped by the heart per minute. This can result in decreased oxygenation of tissues and organs, leading to complications such as heart failure. Nursing Interventions:
- Monitor the patient’s blood pressure and heart rate regularly.
- Assess for signs and symptoms of decreased cardiac output, such as shortness of breath, fatigue, and edema.
- Administer medications as prescribed to manage hypertension and improve cardiac function.
Rationale: These interventions aim to prevent complications related to decreased cardiac output and promote optimal cardiac function.
Ineffective Tissue Perfusion
Hypertension can also lead to ineffective tissue perfusion, which refers to the inadequate delivery of oxygen and nutrients to tissues and organs. This can result in tissue damage and organ dysfunction. Nursing Interventions:
- Monitor the patient’s blood pressure and assess for signs and symptoms of inadequate tissue perfusion, such as decreased urine output and cool, clammy skin.
- Administer medications as prescribed to manage hypertension and improve tissue perfusion.
- Encourage the patient to maintain a healthy lifestyle to improve overall circulation.
Rationale: These interventions aim to prevent complications related to ineffective tissue perfusion and promote optimal tissue perfusion.
Risk for Impaired Renal Perfusion
Hypertension can also lead to impaired renal perfusion, which refers to the inadequate delivery of blood to the kidneys. This can result in kidney damage and dysfunction. Nursing Interventions:
- Monitor the patient’s blood pressure and assess for signs and symptoms of impaired renal perfusion, such as decreased urine output and elevated creatinine levels.
- Administer medications as prescribed to manage hypertension and improve renal perfusion.
- Encourage the patient to maintain a healthy lifestyle to improve overall renal function.
Rationale: These interventions aim to prevent complications related to impaired renal perfusion and promote optimal renal function.
Anxiety
Patients with hypertension may experience anxiety related to their diagnosis and the potential complications associated with it. Nursing Interventions:
- Assess the patient’s anxiety level and provide emotional support as needed.
- Educate the patient on hypertension and its management to alleviate anxiety and promote understanding.
- Refer the patient to a mental health professional if necessary.
Rationale: These interventions aim to alleviate anxiety related to hypertension and promote patient understanding and coping skills.
Hypertension Nursing Interventions
1. Encourage Lifestyle Modifications
Encouraging lifestyle modifications is an essential nursing intervention for patients with hypertension. Nurses should educate patients on the importance of lifestyle changes such as reducing salt intake, increasing physical activity, and maintaining a healthy weight. The following are some nursing interventions for encouraging lifestyle modifications:
- Assess the patient’s current lifestyle and identify areas that need improvement.
- Provide educational materials on healthy lifestyle habits and hypertension management.
- Collaborate with other healthcare professionals to develop a personalized plan for the patient.
- Monitor the patient’s progress and provide positive reinforcement for successful lifestyle changes.
2. Administer Medications as Prescribed
Administering medications as prescribed is crucial in managing hypertension. Nurses should be knowledgeable about the medications used to treat hypertension and their potential side effects. The following are some nursing interventions for administering medications:
- Administer medications as prescribed by the healthcare provider.
- Monitor the patient for any adverse reactions to the medication.
- Provide education on the importance of medication compliance and potential side effects.
- Collaborate with the healthcare provider to adjust medication dosages as needed.
3. Monitor Vital Signs and Cardiac Output
Monitoring vital signs and cardiac output is essential in managing hypertension. Nurses should be skilled in assessing vital signs and interpreting cardiac output measurements. The following are some nursing interventions for monitoring vital signs and cardiac output:
- Assess the patient’s blood pressure, heart rate, and respiratory rate on a regular basis.
- Monitor the patient’s cardiac output using non-invasive methods such as echocardiography or electrocardiography.
- Report any significant changes in vital signs or cardiac output to the healthcare provider.
- Collaborate with the healthcare provider to adjust medication dosages or other interventions as needed.
4. Monitor Renal Function
Monitoring renal function is crucial in managing hypertension. Nurses should be knowledgeable about the impact of hypertension on renal function and the potential complications that can arise. The following are some nursing interventions for monitoring renal function:
- Assess the patient’s renal function using laboratory tests such as serum creatinine and blood urea nitrogen.
- Monitor the patient’s urine output and report any significant changes to the healthcare provider.
- Provide education on the importance of maintaining good renal function and potential complications of hypertension on renal function.
- Collaborate with the healthcare provider to adjust medication dosages or other interventions as needed.
5. Provide Emotional Support
Providing emotional support is essential in managing hypertension. Patients with hypertension may experience anxiety, depression, or other emotional issues related to their condition. The following are some nursing interventions for providing emotional support:
- Assess the patient’s emotional state and provide support as needed.
- Provide education on stress management techniques such as deep breathing, meditation, or yoga.
- Refer the patient to a mental health professional if needed.
- Collaborate with the healthcare team to provide comprehensive care for the patient.
Rationales
Promote Compliance with Treatment Regimen
Patients with hypertension often struggle to adhere to their treatment regimen due to various reasons such as forgetfulness, cost, side effects, and lack of understanding.
By promoting compliance with treatment regimen, nurses can help patients achieve better blood pressure control and reduce the risk of complications.
Nurses can educate patients on the importance of taking medications as prescribed, monitoring blood pressure at home, and attending follow-up appointments. Providing written instructions, pill organizers, and reminders can also improve compliance.
Decrease Blood Pressure and Risk of Complications
The ultimate goal of hypertension management is to decrease blood pressure and prevent complications such as heart attack, stroke, and kidney damage.
Nurses can implement various interventions to achieve this goal, such as administering antihypertensive medications, monitoring blood pressure regularly, and encouraging lifestyle modifications such as exercise, healthy diet, and stress reduction. Nurses can also educate patients on the signs and symptoms of complications and when to seek medical attention.
Detect and Treat Complications Early
Despite optimal management, some patients may develop complications related to hypertension. Nurses can play a critical role in detecting and treating complications early to prevent further damage. For example, nurses can monitor for signs of heart failure, stroke, and renal failure, and intervene promptly by administering medications, oxygen therapy, or dialysis.
Nurses can also educate patients on the importance of self-monitoring and reporting any changes in symptoms.
Prevent Renal Failure
Hypertension is a leading cause of renal failure, which can have devastating consequences for patients. Nurses can implement interventions to prevent renal failure, such as monitoring kidney function regularly, administering medications to control blood pressure and blood sugar, and encouraging patients to maintain a healthy lifestyle.
Nurses can also educate patients on the importance of avoiding nephrotoxic medications and reporting any changes in urine output or color.
Reduce Anxiety and Promote Coping Skills
A diagnosis of hypertension can be overwhelming and anxiety-provoking for patients. Nurses can help reduce anxiety and promote coping skills by providing emotional support, educating patients on the nature of hypertension and its management, and encouraging patients to engage in self-care activities such as meditation, deep breathing, and relaxation techniques.
Nurses can also refer patients to support groups or mental health professionals as needed.
Frequently Asked Questions
- What are the risk factors for hypertension?
The risk factors for hypertension include age, family history, obesity, sedentary lifestyle, smoking, excessive alcohol consumption, stress, and underlying medical conditions such as diabetes, kidney disease, and sleep apnea.
- What are the signs and symptoms of hypertension?
Hypertension is often referred to as the “silent killer” because it typically does not cause any symptoms until it reaches an advanced stage.
However, some patients with hypertension may experience symptoms such as headache, dizziness, nosebleeds, chest pain, or shortness of breath. In severe cases, patients may also experience confusion, vision changes, or seizures.
- What is the nursing management for patients with hypertension?
The nursing management for patients with hypertension includes assessing and monitoring the patient’s blood pressure, providing education on lifestyle modifications such as diet and exercise, administering medications as prescribed, monitoring for side effects and complications of medications, and assisting with referral to appropriate healthcare providers such as a primary care physician, cardiologist, or nephrologist.
The nurse should also educate the patient and family about the condition, provide emotional support, and assist with discharge planning and follow-up care.
Nursing References
Ackley, B. J., Ladwig, G. B., Makic, M. B., Martinez-Kratz, M. R., & Zanotti, M. (2020). Nursing diagnoses handbook: An evidence-based guide to planning care. St. Louis, MO: Elsevier. Buy on Amazon
Gulanick, M., & Myers, J. L. (2022). Nursing care plans: Diagnoses, interventions, & outcomes. St. Louis, MO: Elsevier. Buy on Amazon
Ignatavicius, D. D., Workman, M. L., Rebar, C. R., & Heimgartner, N. M. (2018). Medical-surgical nursing: Concepts for interprofessional collaborative care. St. Louis, MO: Elsevier. Buy on Amazon
Silvestri, L. A. (2020). Saunders comprehensive review for the NCLEX-RN examination. St. Louis, MO: Elsevier. Buy on Amazon
Disclaimer:
Please follow your facilities guidelines, policies, and procedures.
The medical information on this site is provided as an information resource only and is not to be used or relied on for any diagnostic or treatment purposes.
This information is intended to be nursing education and should not be used as a substitute for professional diagnosis and treatment.